 The nasal OCT device provides high resolution images of the cilia in the airway.A paper published today in Science Translational Medicine describes a simple, minimally invasive new tool for viewing differences in the nasal airways of cystic fibrosis patients in vivo at a cellular level. The new technique provides high-resolution images of the hair-like structures called cilia that line nasal airways as well as of the detailed features of the clearance of mucus, which is impaired in people with CF, causing significant morbidity.
The nasal OCT device provides high resolution images of the cilia in the airway.A paper published today in Science Translational Medicine describes a simple, minimally invasive new tool for viewing differences in the nasal airways of cystic fibrosis patients in vivo at a cellular level. The new technique provides high-resolution images of the hair-like structures called cilia that line nasal airways as well as of the detailed features of the clearance of mucus, which is impaired in people with CF, causing significant morbidity.
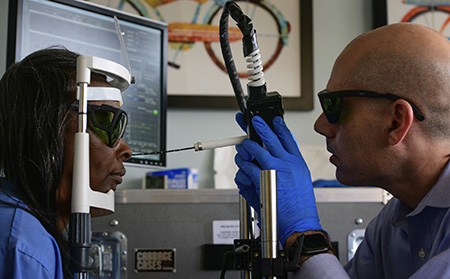
The imaging catheter, which is about 2 mm in diameter, uses optical coherence tomography with a resolution of about 1 micrometer — a 50th the size of a human hair — allowing researchers to probe the nasal passages of patients without even sedating them.
“We’ve done a lot of benchtop imaging with micro-OCT, but this is the first time we’ve been able to use it in people,” said co-principal investigator Guillermo Tearney, M.D., Ph.D., a pathologist and investigator for the Department of Pathology and Wellman Center for Photomedicine at Massachusetts General Hospital, the Remondi Family MGH Research Institute Chair, and professor of pathology at Harvard Medical School. “It’s unprecedented to see this pathophysiology dynamically in living patients. It will allow us to begin to understand things we never even knew were there.”
|
"Now we’ll be able to see how various treatments — not only those intended to fix the mucus, but also agents that repair the basic CF defect — affect airways.” |
Among the researchers’ findings were that, in CF patients, the mucus was dehydrated and moved slowly, impacting cilia speed. The mucus also contained more inflammatory cells. There were other surprises, though, like that they could measure that mucus was more viscous, and patches of CF patients’ cilia and epithelium were ablated.
“We thought they were there but just not functioning well,” Tearney said, “but in places, they were just completely gone.”
The approximately 30,000 cystic fibrosis patients in the United States have an average life expectancy of over 45 years. The new technique will allow clinicians to diagnose and monitor diseases that affect the airways earlier and optimize drug therapies for CF patients.
“Visualizing abnormal mucus will be a powerful tool,” said co-principal investigator Steven M. Rowe, M.D., director of the Gregory Fleming James Cystic Fibrosis Research Center and a professor of medicine at the University of Alabama at Birmingham. “Now we’ll be able to see how various treatments — not only those intended to fix the mucus, but also agents that repair the basic CF defect — affect airways.”
 Developed for use with CF patients, the device might be useful for other respiratory diseases and as a screen for GI disease.The researchers expect micro-OCT to have many applications beyond cystic fibrosis — from diagnosing and treating respiratory ailments like primary ciliary dyskinesia, chronic sinus disease and chronic obstructive pulmonary disease to screening the GI tract for diseases and imaging coronary artery cells.
Developed for use with CF patients, the device might be useful for other respiratory diseases and as a screen for GI disease.The researchers expect micro-OCT to have many applications beyond cystic fibrosis — from diagnosing and treating respiratory ailments like primary ciliary dyskinesia, chronic sinus disease and chronic obstructive pulmonary disease to screening the GI tract for diseases and imaging coronary artery cells.
“The goal is to figure out who else it can be used to help,” Rowe said, “and make it more broadly accessible as a device.”
The paper was a culmination of a 10-year collaboration between Rowe and Tearney. Co-authors of the Science Translational Medicine paper are Hui Min Leung of Harvard Medical School and the Wellman Center for Photomedicine at MGH; Chulho Hyun, Timothy N. Ford and Justin H. Palermo, also of the Wellman Center; Susan E. Birket, George M. Solomon, Ren-Hay Shei, Adegboyega Timothy Adewale, Andrew R. Lenzie, Courtney M. Fernandez-Petty, Do-Yeon Cho and Bradford A. Woodworth, of the UAB Gregory Fleming James Cystic Fibrosis Research Center; Hui Zheng of Harvard Medical School and MGH’s Biostatistics Center; Dongyao Cui of Nanyang Technological University in Singapore; and Lael M. Yonker and Bryan P. Hurley of MGH’s Mucosal Immunology and Biology Research Center.