Researchers at the University of Alabama at Birmingham (UAB) School of Public Health say a 10-millimeter difference in blood pressure is associated with an 8 percent increase in stroke risk for white people, but a 24 percent increase in stroke risk for black people.
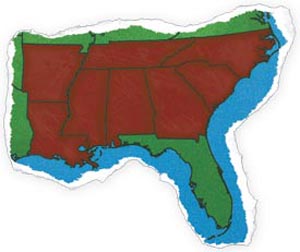 |
| The study’s aim is to determine reasons for higher stroke death rates in the “Stroke Belt” stretching across Alabama, Arkansas, Louisiana, Mississippi, North Carolina, South Carolina, Georgia, and Tennessee. (UAB Magazine) |
Department of Biostatistics professor George Howard, Dr.P.H, said these new findings, recently published online in the Archives of Internal Medicine, mean primary care physicians should work closely with their black patients and urge them to take blood pressure medicine, as well as follow up with them to ensure those medications are effective in bringing blood pressure under control.
“It’s long been hypothesized that hypertension is one of the major drivers in the racial disparities with stroke,” Howard said. “Blacks between the ages of 45-65 are about three times more likely to have a stroke than their white counterparts. The reasons for that were not understood, but this difference is bigger than can be explained simply by the fact that more blacks have high blood pressure. There must be something else going on.”
The discovery was part of the long-running REGARDS (Reasons for Geographic and Racial Differences in Stroke) study, led by Howard. Stroke risk was assessed in 30,329 black and white people ages 45 and older enrolled in REGARDS between 2003 and 2007 — 27,748 were included in this most recent analysis and followed up with through 2011.
| The discovery was part of the long-running REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. |
Howard says that when these racial differences in the impact of blood pressure levels are coupled with previous REGARDS findings that showed a higher prevalence of hypertension and poorer control of hypertension in blacks, it contributes important information to explaining the racial disparity in stroke risk.
Howard noted that at blood pressures above 140, black REGARDS participants had a 400 percent higher chance of having a stroke, compared with white participants. At pressures of 120 or below, white participants had a higher stroke risk.
According to Howard, the public health burden of the racial disparities in stroke is costly. Having a stroke is expensive — to the tune of $140,000 — and the extra strokes in blacks cost $3 billion per year.
“These racial disparities, along with geographic disparities, have been in existence and clearly documented for nearly 60 years,” Howard said. “We hope the findings from this study will be used to develop new interventions to reduce these disparities.”
In the stroke belt states — Alabama, Arkansas, Georgia, Louisiana, Mississippi, North Carolina, South Carolina and Tennessee — the risk of dying from stroke is higher than in other parts of the country. In Alabama, the stroke death rate is 105.5 per every 100,000 people, compared with a national average of 78.6 per 100,000. For blacks in the stroke belt, the death rate is 146.4 per 100,000, compared to the national average for all blacks of 116.4 per 100,000. For whites in the stroke belt, the rate is 96.4 per 100,000, compared to the national average for all whites of 77.1 per 100,000.