A triple-combination drug has been shown to be effective in markedly improving lung function for the majority of patients with cystic fibrosis. The new triple therapy should provide therapeutic benefits for 90 percent of all patients with the genetic disease.
In findings published in the New England Journal of Medicine and presented today at the North American Cystic Fibrosis Conference in Denver, researchers from the University of Alabama at Birmingham report that the medication, which combines an experimental compound known as VX-659 with two existing medications, tezacaftor and ivacaftor, improved lung function by more than 12 percent compared to placebo. VX-659, along with tezacaftor and ivacaftor, was developed by Vertex Pharmaceuticals.
 Click to enlarge. Credit: Cystic Fibrosis FoundationThe current findings come on the heels of research presented by the same investigators in November 2017 that showed the combination of tezacaftor and ivacaftor produced a substantial improvement in lung function in CF patients with a particular set of mutations in the CFTR gene responsible for the disease, accounting for about 15 percent of all those with CF. This two-drug combination also helped patients with two copies of the most common mutation, termed Phe508del, which is responsible for CF in about 50 percent of cases, but the benefit was more modest.
Click to enlarge. Credit: Cystic Fibrosis FoundationThe current findings come on the heels of research presented by the same investigators in November 2017 that showed the combination of tezacaftor and ivacaftor produced a substantial improvement in lung function in CF patients with a particular set of mutations in the CFTR gene responsible for the disease, accounting for about 15 percent of all those with CF. This two-drug combination also helped patients with two copies of the most common mutation, termed Phe508del, which is responsible for CF in about 50 percent of cases, but the benefit was more modest.
The addition of VX-659 provided a substantially greater benefit in improved lung function for that group of patients. Additionally, it improved lung function in another 30 percent of patients with only one copy of the common Phe508del mutation, a group that had not responded to the ivacaftor/tezacaftor combination alone.
“Ivacaftor was the first medication to treat the underlying cause of CF, and it was a major breakthrough for that small group of patients when it was introduced in 2012,” said Steven Rowe, M.D., director of the Gregory Fleming James Cystic Fibrosis Center, professor in the Division of Pulmonary, Allergy and Critical Medicine at UAB, and communicating author of the study. “Last year’s announcement of the combination therapy of ivacaftor and tezacaftor was another major step. Today’s findings of the triple combination’s effectiveness indicates that we are now even closer to having meaningful therapy for nearly all those with cystic fibrosis.”
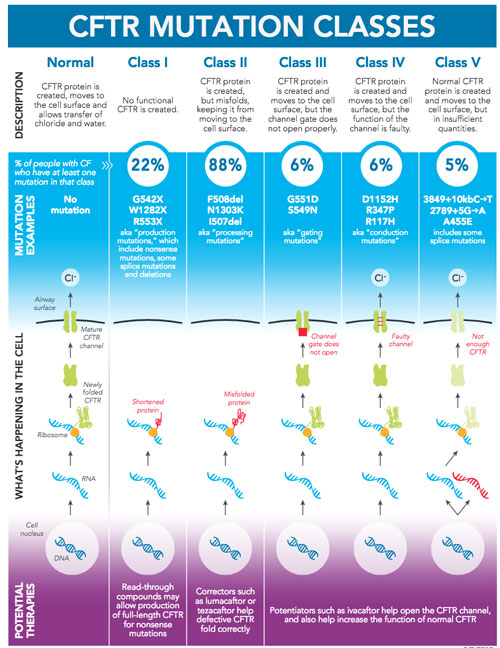
Cystic fibrosis is caused by any one of several defects in the CFTR protein, which regulates fluid flow through cells and affects the components of lung mucus, digestive fluids and sweat. In a healthy cell, salt and fluid pass through the CFTR ion channel to the cell surface. To achieve this, the CFTR protein must undergo a complex process known as protein folding to assume the proper shape. A hallmark of the most common form of CF is misfolded proteins that cannot pass through the ion channel to the cell’s surface.
Tezacaftor and the new compound VX-659 are known as CF correctors. Their role is to help mutant CFTR proteins fold properly. Ivacaftor is a potentiator, serving to activate CFTR to help keep the ion channel open. In combination, the three work to improve overall lung function by restoring proper operation of the CFTR ion channel, allowing salt and fluid to pass into the airways more normally.
Related article: |
| After a cystic fibrosis 'miracle,' researchers are exploring ways to reach millions more |
The UAB-led Phase II study looked at 115 patients at 48 sites in the United States, United Kingdom, Ireland and Israel. A second study, also presented today and communicated by investigators at the University of Colorado, presented similar findings of a second experimental compound, VX-445, used in conjunction with ivacaftor and tezacaftor.
“When we presented our findings last year that ivacaftor and tezacaftor worked well in combination, we were extremely excited, as we knew that these next-generation medications — VX-659 and VX-445 — were in development and depended upon that success,” Rowe said. “The current discoveries represent a tremendous step toward creating a treatment strategy that could provide highly effective CFTR modulation therapy for the vast majority of patients with CF.”
Rowe says large-scale, Phase III studies of the triple combination therapies are already underway. Successful completion of a Phase III study is the last step before submission to the Food and Drug Administration for approval to bring a medication to market.
According to Rowe, patients on the triple-combination therapy found it easier to breathe and enjoyed a greater quality of life. While the study did not assess a change in life expectancy, Rowe says it is likely that, if further development is successful, the drug will help push average life expectancy, currently around 47 years of age, even higher.
Side effects and adverse events reported in the study were mostly mild and well-managed.
Rowe holds the Nancy R. and Eugene C. Gwaltney Family Endowed Chair in Medical Research at UAB. Funding for the study was provided by Vertex Pharmaceuticals, and earlier development costs were provided by the Cystic Fibrosis Foundation. Infrastructure funding was provided by the National Institutes of Health, the UAB School of Medicine, and the UAB Center for Clinical and Translational Science.