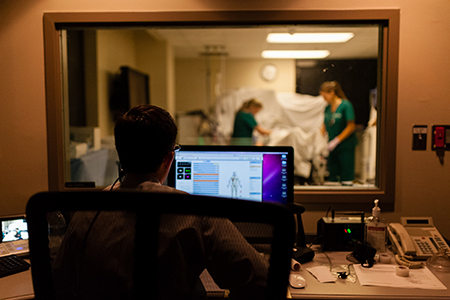
One patient is having trouble breathing. A new mom is experiencing bleeding. Another patient is having complications from his diabetes. Labs are being run. The intensive-care unit is buzzing with activity.
One patient is having trouble breathing. A new mom is experiencing bleeding. Another patient is having complications from his diabetes. Labs are being run. The intensive-care unit is buzzing with activity.
Behind the scenes, professors and volunteers are in a control room manipulating manikins and monitors. This isn’t a normal day in the ICU; it’s a simulation designed to test UAB health-care students’ ability to communicate effectively and provide better patient care.
“Simulations such as this provide students an opportunity to both test what they have learned and to collaborate within the health-care team, said Penni Watts, R.N., instructor in nursing and faculty lead for the simulation. “The simulated setting allows students to demonstrate their patient care skills before practicing on real patients.”
“We expect students to know how to deal interprofessionally once they enter their hospital setting, but we never teach them how to do that,” said Kevin Leon, M.D., associate professor of medicine. “This teaches them how to communicate with each other and how to ask for help when appropriate.”
The Intensive Care Unit Interprofessional Education simulation is organized through the Office of Interprofessional Simulation for Innovative Practice (OIPS) and developed by faculty from the schools of Nursing, Health Professions and Medicine and staff in the UAB Center for Patient Safety and Advanced Medical Simulation. More than 190 students from seven professions participated in one of six two-hour sessions during the two-day simulation event that employed manikins and standardized patients.
“All simulations follow a similar format,” said Marjorie Lee White, M.D., interim co-director of OIPS, director of medical student simulation and associate professor of pediatrics. “Participants receive a pre-briefing, which contains information to set them up for success. They care for six complex patients who will have myriad medical conditions and then participate in a structured debriefing.”
White said the debriefing provides students time to reflect on their feelings, behaviors and actions as a member of the health-care team. She said students report that most of their learning occurs during the debriefing.
 Emphasis on teamwork, in health care and all academic disciplines, is the centerpiece of the UAB Quality Enhancement Plan. The QEP is a requirement of the Southern Association of Colleges and Schools Commission on Colleges, designed to improve an aspect of student learning and enhance the quality of higher education.
Emphasis on teamwork, in health care and all academic disciplines, is the centerpiece of the UAB Quality Enhancement Plan. The QEP is a requirement of the Southern Association of Colleges and Schools Commission on Colleges, designed to improve an aspect of student learning and enhance the quality of higher education.
“The QEP theme of teamwork fits seamlessly within the objectives of simulations such as the Intensive Care Unit Interprofessional Simulation as patient care, particularly that in an intensive-care unit, is delivered in teams,” White said.
“From a laboratory perspective, it’s important for our students to be able to see what’s going on at the bedside and what’s happening clinically, because often the laboratory is off site,” said Michelle Brown, assistant professor of clinical laboratory science. “Sometimes you can be desensitized from what’s really going on, and involving students in a high-acuity patient situation helps them remember what’s on the other side of that specimen.”
Brown said simulations also are important in assessing students’ abilities and revealing areas that need to be re-addressed in class. She said she already has seen an opportunity for improvement: Students took a long time to get blood ready during a urgent transfusion, so she will review that again in class.
“For each individual profession, this is a safe environment to practice their skills without feeling worry or concern they’re doing something wrong that will harm patients,” Leon said. “The students can work through some of their anxiety here before they’re dealing with real patients, which is extremely helpful.”
Elizabeth Sanford, a second-year student in the doctor of physical therapy program, said simulations help her to feel more comfortable in her role on the health-care team.
“When something is outside the scope of my practice, I know I can call on somebody else to be there,” Sanford said. “It helps you appreciate all of the other aspects of the health-care team.”
Leon said the simulation also helps students learn about the knowledge and skills students in the other professions have. “They really don’t know what these other professions can do,” Leon said. “Most of our positive feedback is about how the students are dealing with each other and how helpful that was.”
Jerry King, interim director of the respiratory therapy program, said the simulation is the only opportunity to function without a professor standing over their shoulder.
“Next month at this time, respiratory therapy students will be doing this in a real-world setting,” King said. “We’d rather them make a mistake on the manikin so they can learn from it in a safe way.”
Kaylee Gunn, student in the Accelerated Master’s in Nursing Pathway program, said she thought the simulation was valuable in demonstrating the demands of a job in an intensive-care unit.
“This is giving us the opportunity to see firsthand what our responsibility is going to be as soon as we come out of the nursing program, become and RN and get a job,” Gunn said. “I can sit in class all day and hear about what my role is and what my responsibilities are, but to actually do them is much better.”