{slide=Introduction}
- The 2011 ATS/ERS/JRS/ALAT guidelines list a number of recommendations for the diagnosis and clinical management of patients with IPF
- The level of understanding and adherence to the guidelines among non-academic practicing pulmonologists is limited
- The UAB “bundle of care” identifies specific measures drawn from the 2011 guidelines to help address this gap
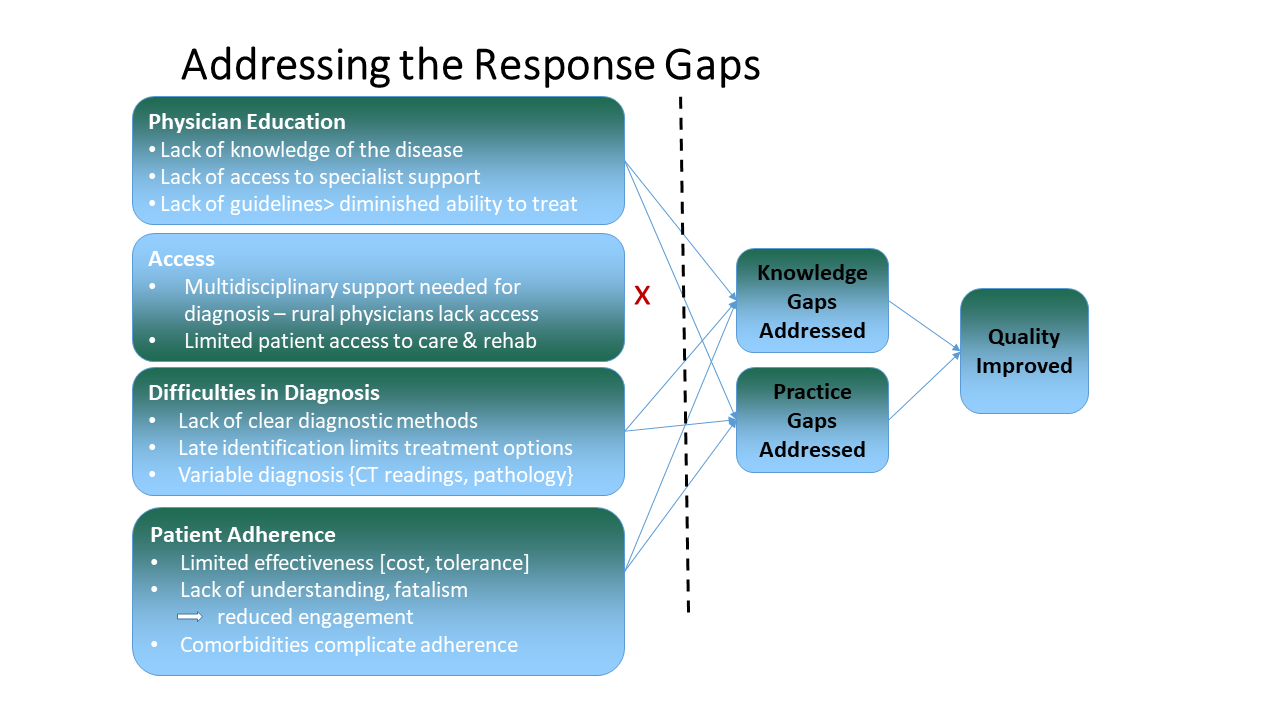
- This project sought to address the practice gaps and barriers to optimal management of patients with IPF through:
- Identifying specific education needs through nominal groups,
- developing education based on those needs, and
- measuring specific practice change, based on the UAB bundle of care, following completion of the education activity
{slide=Objectives & Methods}
Objectives
- Increase delivery of evidence-based care in accordance with expert guideline recommendations at the physician, team, and practice level
- Communicate best practices in the management of patients with IPF that allows physicians to compare their own clinical performance with expert guidelines
- Increase the percentage of patients with IPF appropriately managed and monitored, based on the expert guideline recommendations
Methods
- Community pulmonologists provide perspective on central question.
- baseline data related to bundle-of-care measures collected
- Pulmonologists complete an education intervention and post-test that addressed the issues prioritized by the nominal groups
- A follow-up visit compare pre- and post-intervention performance on the bundle-of-care measures
{slide=Process/Results}
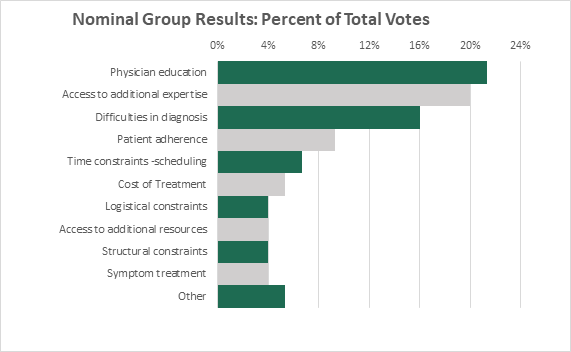
Physician provided and discussed responses to this question:
From your perspective, as a clinician, what are the barriers to achieving optimal care of patients with IPF?
| Group Session | # Participants | # Items | # Items Ranked | In-session Votes | Weighted Votes |
| Group #1 | 6 | 20 | 16 | 30 | 90 |
| Group #2 | 6 | 15 | 13 | 30 | 90 |
| Group #3 | 3 | 15 | 9 | 15 | 45 |
| Total | 15 | 50 | 38 | 75 | 225 |
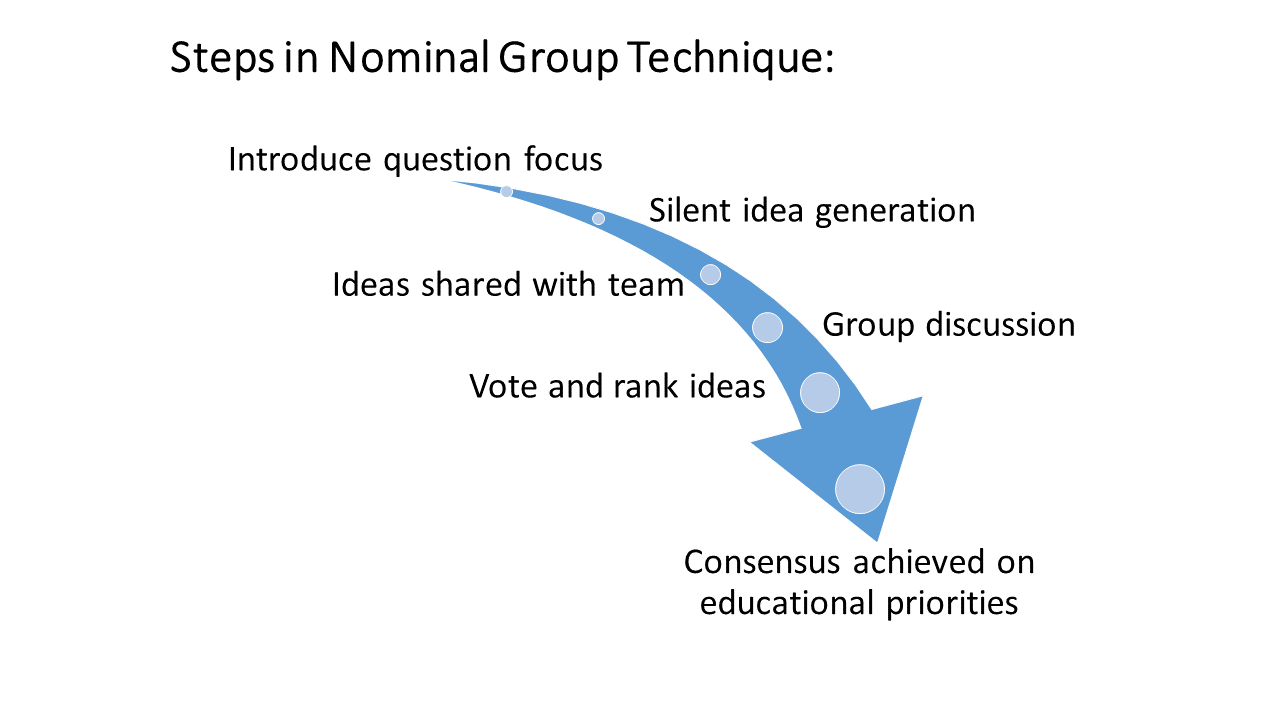
- All participants contribute responses to the question
- Responses captured verbatim
- Process continues until group feels all significant ideas are captured
- Each participant selects and ranks five of the items contributed
- Group reviews and evaluates results
- 3 raters identified most critical themes, actionable themes incorporated into education content
{/slide}
{slide=Process/Results, continued}
Actionable themes: Improve physician basic knowledge; Reduce barriers to diagnosis; improve physician-physician and physician-patient communication
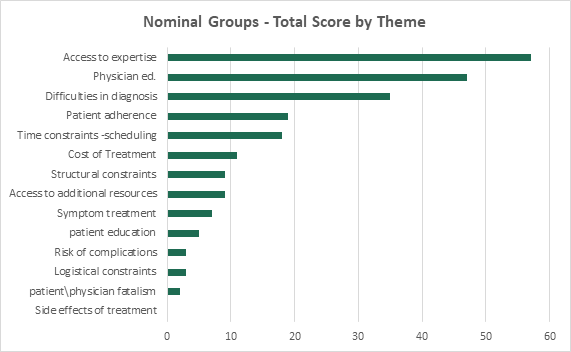
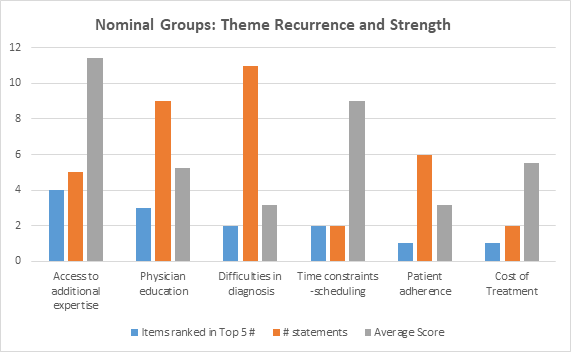
- Top 5 Score Identifies items that the groups feel most strongly about
- Number Score How often participants refer to a theme or issue
- Average Score Standardizes the score for each theme
{/slide}
{slide=Conclusions}
Nominal Groups Key Findings:
- Diagnosis of IPF: Need for earlier inclusion of IPF in the differential diagnosis of a patient presenting with dyspnea, cough, and crackles in lung auscultation
- include appropriate protocol for performing and interpreting HRCT
- Diagnosis of IPF: Information on when to consider a surgical lung biopsy
- Management of IPF: Symptom management, including control of cough, referral to palliative care and rehabilitation
- Management of IPF: When to consider anti-fibrotic therapy with nintendanib or pirfenidone; how to monitor for safety/adverse events, when to stop/switch therapies
Post-Intervention Performance
- Increased percentage of eligible patients who were treated with pirfenidone or nintedanib (20% at baseline and 46% at follow up)
- Increased percentage of patients who had routine clinic visits with PFTs at least once within the past 6 months (40% at baseline and 64% at follow up)
- Increased percentage of patients who were monitored for exercise-induced hypoxemia with a 6MWT or equivalent at least once in the past 6 months (7% at baseline, and 36% at follow up)
{/slide}