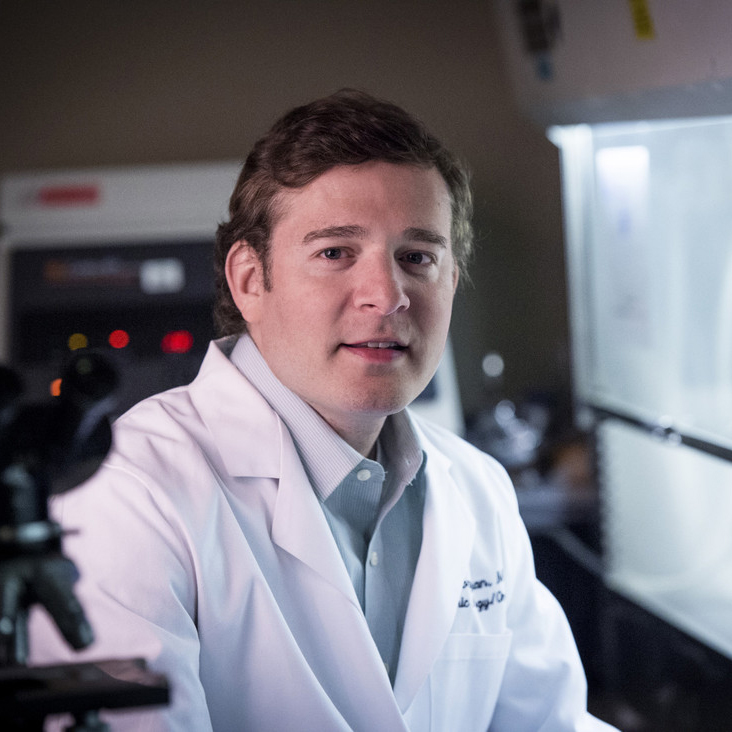
 Gregory Friedman, M.D., professor in the Department of Pediatrics, is the latest winner of the School of Medicine’s Featured Discovery. This initiative celebrates important research from School of Medicine faculty members.
Gregory Friedman, M.D., professor in the Department of Pediatrics, is the latest winner of the School of Medicine’s Featured Discovery. This initiative celebrates important research from School of Medicine faculty members.
Friedman, the lead Principal Investigator, and his multi-institutional team were recently published in New England Journal of Medicine for their paper “Oncolytic HSV-1 G207 Immunovirotherapy for Pediatric High-Grade Gliomas.”
About the study, Friedman says, “We greatly need effective and less-toxic, targeted therapies for children with progressive malignant brain tumors, as outcomes are very poor and toxicities caused by current standard therapies are unacceptably high.”
To date, immunotherapies have been ineffective in treating pediatric brain tumors because the tumors are typically immunologically ‘cold’ with very few immune cells present that are required for an immune attack on the tumor.
Friedman’s team, which was collaborative between UAB and Children’s of Alabama, led a first-in-children investigator-initiated Phase 1 trial to test the safety of an immunotherapy using an altered cold-sore virus (HSV-1), G207, infused via catheters and placed directly into progressive or recurrent pediatric high-grade gliomas.
Due to modifications in the virus, G207 does not harm normal cells but can infect and directly kill tumor cells while also stimulating the patient’s own immune system to attack the tumor.
“We found that G207 was very safe with only mild and infrequent side effects, and we discovered that the therapy turned ‘cold’ tumors to ‘hot' by resulting in a striking infiltration of immune cells into the tumors,” Friedman explains.
The therapy led to a 120% increase in the median overall survival compared to historical data. “While the results are promising, we will need to confirm them in an upcoming Phase 2 trial,” Friedman says.
Friedman was recently awarded a grant to begin Phase 2 from the Rally Foundation for Childhood Cancer Research. Read more about Phase 1 and the upcoming Phase 2 trial from UAB News.
Read the full study in New England Journal of Medicine.
The School of Medicine communications staff sat down with Dr. Friedman to gain insights about the research of this study, UAB, and the science community.
Q: What compelled you to pursue this research?
While overall survival rates for many childhood cancers have improved greatly, unfortunately, outcomes for children with malignant brain tumors have lagged behind other types of cancer. For example, survival rates for pediatric high-grade glioma are <20% and have not improved in 30+ years. Also, children who survive often suffer with lifelong disabilities from current treatments and the disease itself. There is an incredibly great need for novel, targeted, less-toxic therapies for this vulnerable population, and a desire to fulfill that need is what compelled me to pursue this research.
Q: How do you feel your research will impact the science community?
To date, immunotherapies like checkpoint inhibitors, which can release the brakes applied by tumors on the immune system and have been effective in many adult solid tumors, have been ineffective in pediatric solid tumors because pediatric tumors lack immune cells and have a very low mutational burden and fewer mutations than adult tumors. Our findings that oncolytic virotherapy using a modified cold-sore virus is safe and can alter the tumor microenvironment by turning immunologically ‘cold’ pediatric brain tumors to ‘hot’ and stimulating an apparent immune attack on tumors with few mutations, suggest that immunotherapy can be effectively used to target pediatric brain tumors. We anticipate our findings will generate great interest from the scientific community to gain a better understanding of how the tumor microenvironment can be favorably modulated with therapies like oncolytic virotherapy and to devise combination therapies which maximize and maintain the immune attack against pediatric tumors.
Q: What is your research’s relevance to human disease?
Based on the promising results, we are actively developing a Phase 2 multi-institutional trial that our team will lead through the Pediatric Brain Tumor Consortium. We hope this trial will lead to the first-ever approved therapy for pediatric high-grade glioma. In addition, based on our preclinical data which showed that medulloblastoma, the most common malignant pediatric brain tumor, may be even more sensitive to the virotherapy than pediatric high-grade glioma, we have an ongoing first-in-human Phase 1 trial to assess the safety and effectiveness of G207 in recurrent pediatric malignant tumors, like medulloblastoma, that arise in the back of the brain or cerebellum. Also, we plan to test the therapy in combination with checkpoint inhibitors in children with newly diagnosed high-grade glioma because we believe that these patients will be even more likely to respond to the therapy prior to receiving chemotherapy, which can suppress their ability to mount an immune response. Lastly, we are developing and testing various combination therapies with G207 in the lab with the goal of sustaining the immune attack against the tumor, and we will advance the most promising combinations to clinical trials in children with brain tumors and other solid tumors outside the brain.
Q: When did you know you had an important discovery?
While it appeared that the patients were responding to the treatment based on radiographic and clinical findings, it became clear to us that we had an important discovery when we examined matched pre- and post-G207 tumor tissue from four patients and saw a dramatic infiltration of immune cells, indicating a shift from immunologically ‘cold’ to ‘hot’ after treatment. This shift represents a critical step in the development of an effective immunotherapy for pediatric brain tumors.
Q: How has being at UAB and living in Birmingham affected your research?
I moved to Birmingham in 2002 for my pediatrics residency, and I initially thought I would be here for just 3 years. However, once I met the outstanding faculty and staff in the Department of Pediatrics and Division of Pediatric Hematology/Oncology, and learned of the incredible research opportunities in the School of Medicine and the O’Neal Comprehensive Cancer Center, I stayed at UAB for my fellowship and then joined the faculty in 2008. I was fortunate to learn from and work with international leaders and giants in the field of oncolytic virotherapy including Drs. Yancey Gillespie, Jim Markert, and Rich Whitley, who gave me an opportunity to expand upon their research in adult glioblastoma to pediatric cancers. This project was successful because of the exceptional, collaborative research environment at UAB and Children’s of Alabama and the support from the leadership at Children’s of Alabama to conduct this unconventional trial. It was truly a team effort with many other individuals at UAB performing critical roles including study coordinator Kara Kachurak, CRNP; Dr. Jim Johnston, study neurosurgeon; Dr. John Fiveash, study radiation oncologist; Drs. Rong Li, Joshua Bernstock, Prescott Atkinson, Avi Madan-Swain, Inmaculada Aban; and my lab members Li Nan and Drs. Kyung-Don Kang and Stacie Totsch.
