 “The human brain is one of the last great frontiers in biomedicine,” says David Sweatt, Ph.D., the Evelyn F. McKnight Endowed Chair for Learning and Memory in Aging at UAB. “It’s the most complicated thing known to exist.” While scientists and physicians have an intricate understanding of the heart, lungs, kidneys, and other internal organs, the best minds still don’t know everything about the brain. That’s what makes neuroscience both challenging and fascinating, says Sweatt, who also chairs the Department of Neurobiology.
“The human brain is one of the last great frontiers in biomedicine,” says David Sweatt, Ph.D., the Evelyn F. McKnight Endowed Chair for Learning and Memory in Aging at UAB. “It’s the most complicated thing known to exist.” While scientists and physicians have an intricate understanding of the heart, lungs, kidneys, and other internal organs, the best minds still don’t know everything about the brain. That’s what makes neuroscience both challenging and fascinating, says Sweatt, who also chairs the Department of Neurobiology.“We understand a lot about brain anatomy, circuitry, and connections. What we don’t know is how that functions to create thoughts, behaviors, and symptoms,” explains Barton Guthrie, M.D., a UAB neurosurgery professor specializing in neuromodulation. “We know what parts of the brain control speech, emotion, and memory, but we don’t know how it works and how to manage and improve it.”
Deepening knowledge is the primary goal of the proposed federal BRAIN (Brain Research through Advancing Innovative Neurotechnologies) initiative, which aims to help researchers find new ways to treat, cure, and prevent brain disorders. And while the exact scope of the initiative has not yet been defined, Sweatt, Guthrie, and other UAB neuroscientists already are pursuing discoveries with the potential to reshape our understanding of the brain and its countless connections. Here are some of the latest breakthroughs:
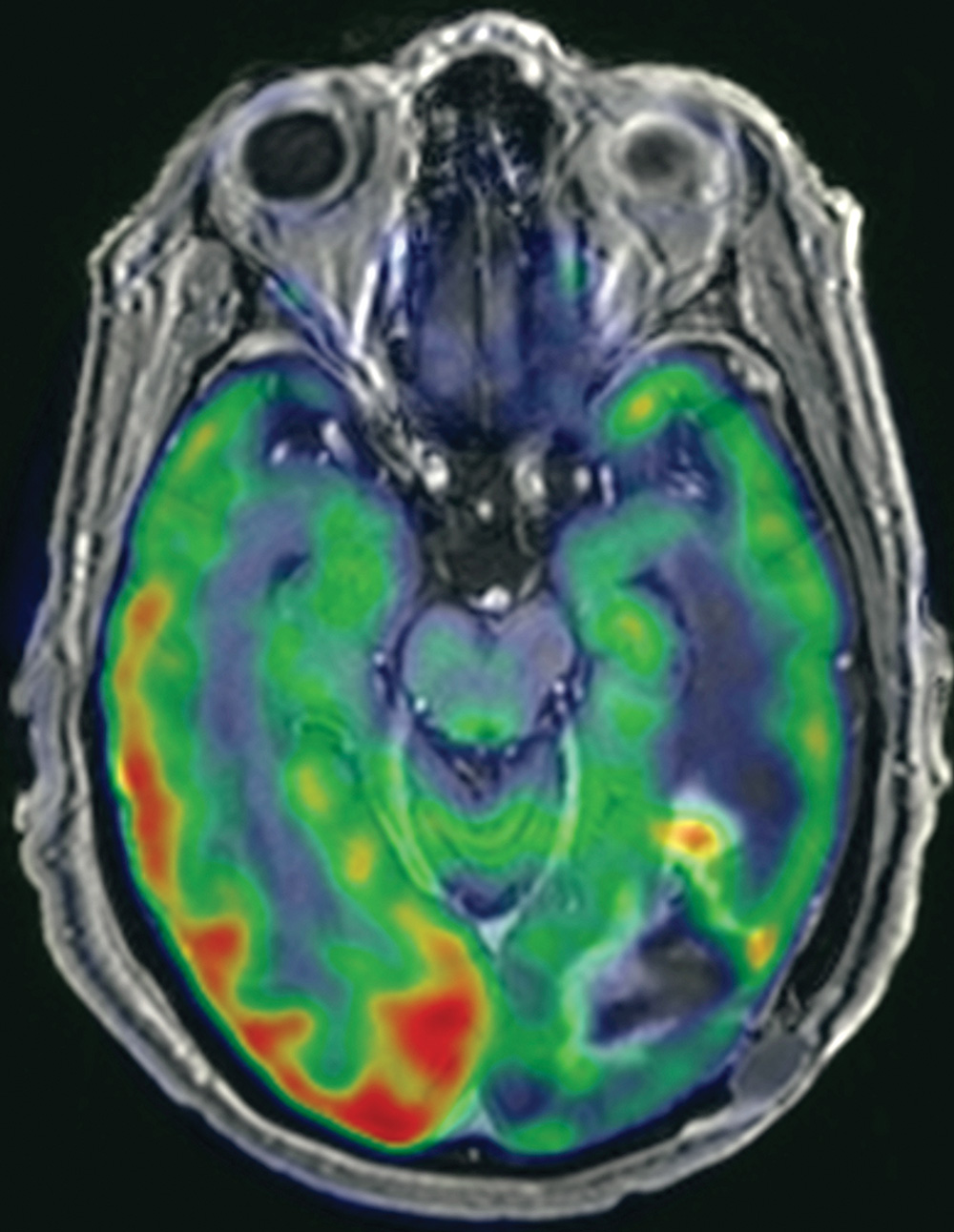
Imaging New Approaches
UAB recently installed a 61,000-pound TR24 cyclotron, part of a new $20-million Advanced Imaging Facility, in the Wallace Tumor Institute. The cyclotron, a particle accelerator that is most powerful of its kind at any academic facility in the country, will provide researchers with better images of the brain as it functions. This could lead to breakthroughs in research for Alzheimer’s and Parkinson’s disease, says David G. Standaert, M.D., Ph.D., the John N. Whitaker Endowed Chair in Neurology and chair of the Department of Neurology.“This moves UAB into the cutting edge of neuroscience,” Standaert explains. “The cyclotron lets us image different chemicals and signaling systems in the brain. More than just the structure of the brain, we’re actually imaging the function and chemistry, which is a tremendously powerful approach. We can start to get a handle on what’s happening with the brain. How is the wiring affected in a disease state? How is the brain compensating? That’s very much in the spirit of the BRAIN initiative.”
Drug Discovery
At the annual meeting of the Society for Neuroscience, Harald Sontheimer, Ph.D, a UAB neurobiology professor and director of both the Center for Glial Biology in Medicine and the Civitan International Research Center, presented his research showing that the FDA-approved drug sulfasalazine can block a transporter in glioma cells that causes seizures. Adrienne Lahti, M.D., director of the UAB’s Division of Behavioral Neurobiology and a psychiatry professor, is now building on this discovery, studying sulfasalazine to see if it can help treat schizophrenia.“In glioma cells, this transporter releases glutamate, causing hyperexcitability in the surrounding neurons,” says Lori McMahon, Ph.D., director of the UAB Comprehensive Neuroscience Center. “One of the things Dr. Lahti examines in her patients is glutamate levels. Her idea is to use sulfasalazine to see if it can relieve seizures.
“Dr. Lahti feels that the brain is completely miswired in schizophrenia. It’s not a single brain region; instead, it’s how the brain works in total. That’s the next big thing that we really need to understand and solve. We’re doing a lot of that kind of research at UAB.”
Attractive Solution
Jerzy Szaflarski, M.D., Ph.D., director of the UAB Epilepsy Center, is conducting a National Institutes of Health study that uses MRIs to examine the brain functions of patients experiencing language problems after strokes. He then employs a technique called transcranial magnetic stimulation in an attempt to improve patient recovery.“He checks to see which areas of the brain are functioning abnormally. Then he induces a magnetic current that can stimulate the brain and actually induce changes,” Standaert says. “So he’s using advanced imaging to sort out not only where the structure is wrong, but also where the function of the brain is wrong, and applying an electrical magnetic approach to try to intervene and correct this.”
Saving Lives on the Front Line
The UAB Department of Psychiatry recently partnered with the UAB Department of Emergency Medicine to study patients who entered the emergency room with severe mood disorders and suicidal thoughts. Some of the patients were given a low dosage of the drug ketamine, an anesthesia medication, while others were given a placebo. Many of the patients who received ketamine began feeling better as quickly as 30 minutes after taking the drug.“The results were dramatic,” says James H. Meador-Woodruff, M.D., the Heman E. Drummond Endowed Chair of Psychiatry and chair of the UAB Department of Psychiatry. “So we’re researching how this works and looking for drugs that can preserve this effect. It has the potential to revolutionize psychiatric care.
“We were the first institution to do this in an inner-city emergency room, and there are still only a couple of other places doing it now. It’s the kind of translational science that I think would fit into the BRAIN initiative. It combines scientists with clinicians on the front line. It’s big science, and it takes a collaborative place like UAB in order to do it.”
This article, written by Cary Estes, originally appeared in the Winter 2014 edition of UAB Medicine Magazine.
