Case History
A 59-year-old female with cystic liver lesion. Prior history of thyroid cancer 17 years ago. What is the diagnosis?
What is the diagnosis?
- Metastatic follicular carcinoma
- Hepatocellular carcinoma
- Papillary mesothelioma
- Metastatic papillary thyroid carcinoma

The answer is “D”, metastatic papillary thyroid carcinoma.
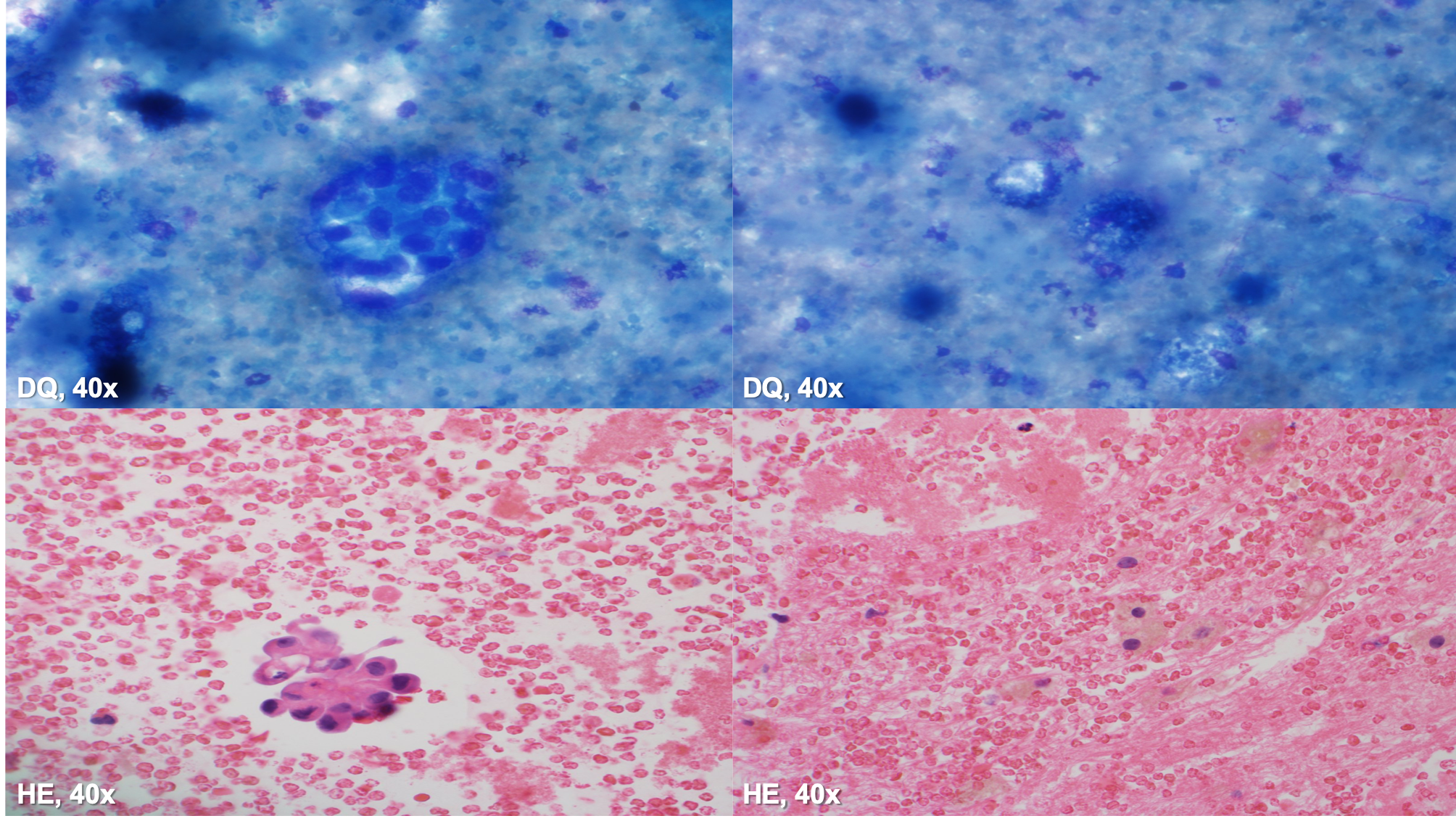
The specimen is hypocellular. The cytopsin is thick but shows some small atypical cell clusters in a background of hepatocytes. The atypical cells are better appreciated in the cellblock, with somewhat enlarged and irregular nuclei, small nucleolus and moderate amounts of eosinophilic cytoplasm.
Immunohistochemical stains were performed on this case. The cells were positive for PAX-8 and TTF-1, and negative for HepPar1, Glypican 3 and Calretinin, consistent with metastatic papillary thyroid carcinoma. The subsequent resection showed a liver cyst with papillary structures, nuclear grooves and chromatin clearing; the cells were also positive for PAX-8 and TTF-1, supporting the original cytologic diagnosis.
Thyroid cancer is the most common malignant endocrine neoplasm in the United States, with papillary thyroid carcinoma (PTC) being the most common primary thyroid cancer. PTC is 2-3 times more common in women than men. PTC classically presents as a painless palpable thyroid nodule, however incidental nodules identified during radiology studies are increasing. Most PTC’s behave in an indolent fashion, but some patients will develop distant metastasis to lung and bone. Liver metastasis from PTC is extremely rare and occurs long after the initial diagnosis.
References
VandenBussche CJ, Gocke CD, Li QK. Fine-needle aspiration of metastatic papillary thyroid carcinoma found in the liver. Diagn Cytopathol. 2013;41(5):418‐424. doi:10.1002/dc.22850