 A national crisis magnifies disparities and inequities in our society. While anyone can be infected by the CoV-SARS-2 virus, the effects of the ongoing pandemic — including the responses from our government and our health care system— do not impact everyone equally. We believe the COVID-19 pandemic is radically exacerbating the deadly consequences of racial and socioeconomic disparities in health and health care in America, creating a crisis within a crisis.
A national crisis magnifies disparities and inequities in our society. While anyone can be infected by the CoV-SARS-2 virus, the effects of the ongoing pandemic — including the responses from our government and our health care system— do not impact everyone equally. We believe the COVID-19 pandemic is radically exacerbating the deadly consequences of racial and socioeconomic disparities in health and health care in America, creating a crisis within a crisis.
We are seeing mounting evidence of pronounced disparities in early reports of how African Americans are weathering the pandemic. In Michigan and Illinois, more than 40 percent of deaths are among African Americans, who make up just 14 percent and 15 percent of their populations, respectively. In Louisiana, African Americans represent 70 percent of deaths, but account for only 33 percent of the state’s population.
These alarming outcomes are in large part the result of longstanding inequities in an array of health determinants, including limited access to health care (especially primary care), and limited access to affordable housing and fresh foods. These have led to higher rates of chronic illnesses like high blood pressure, diabetes and renal failure that increase the risk of severe illness from COVID-19 among minority populations.
As we move forward from this crisis, there must be a renewed commitment to broadly provide health care coverage to the underserved and uninsured, to improve access to housing, and to eliminate food deserts while promoting healthy physical activity in minority and underserved communities.
The COVID-19 pandemic has highlighted just how profoundly health care access and health outcomes are linked with an individual’s employment and income status in the United States. Many African Americans and other minorities cannot stay home because they work in sectors like health care, government, transportation and food supply that are now deemed essential. In cities, minority populations are still riding public transportation in large numbers to go to work, yet another unavoidable exposure risk.
 There is also increasing evidence of disparities in coronavirus testing. In many parts of the country, lack of test kits means a doctor must first refer a patient for testing, and African Americans are less likely to have a primary care physician. Moreover, as reported by National Public Radio, even when African Americans see a physician they may be less likely to be referred for testing, even if they show signs of infection. In certain cities, testing facilities have been concentrated in predominantly white areas. They may be drive-through-only or not on public transportation routes, making them less accessible for people who do not own an automobile.
There is also increasing evidence of disparities in coronavirus testing. In many parts of the country, lack of test kits means a doctor must first refer a patient for testing, and African Americans are less likely to have a primary care physician. Moreover, as reported by National Public Radio, even when African Americans see a physician they may be less likely to be referred for testing, even if they show signs of infection. In certain cities, testing facilities have been concentrated in predominantly white areas. They may be drive-through-only or not on public transportation routes, making them less accessible for people who do not own an automobile.
When resources are limited, those with the most influence and means in a society have vastly greater access to them than the underprivileged and underserved. That is why we must continue to refine our governmental and health care responses to the pandemic to:
- Broadly record and report demographic data on virus spread and mortality. This data is critical to mobilize resources to the hardest-hit, most underserved areas.
- Ensure access to current and emerging therapies and clinical trials. Minorities account for fewer than 10 percent of patients enrolled in clinical trials. We recommend using patient navigators and community health workers to enhance diversity in enrollment.
- Provide mobile access testing sites for vulnerable urban and rural communities. People in these areas need either transportation or on-site testing.
- Communicate with these communities through trusted local stakeholders and leaders. Establish leadership groups to sustain vital involvement from the health care community in these neighborhoods.
- Commit and organize nationally, regionally and locally to address the medical and social determinants of health that have created and sustained the preexisting COVID-19 health disparities.
At this moment of crisis for our country, it is instructive to remember this passage from Dr. Martin Luther King Jr.’s epic Letter from a Birmingham Jail: “It really boils down to this: that all life is interrelated. We are all caught in an inescapable network of mutuality, tied into a single garment of destiny. Whatever affects one destiny, affects all indirectly.”
We must make every effort to protect our most vulnerable communities both during and after this pandemic. That means equal access to testing and appropriate medical care, and equitable investment to help these communities recover physically and economically once the crisis is over. If we fail to address the unique needs and concerns of vulnerable populations, when the coronavirus pandemic finally recedes, we may find that these communities have paid an unthinkable price for our inaction.
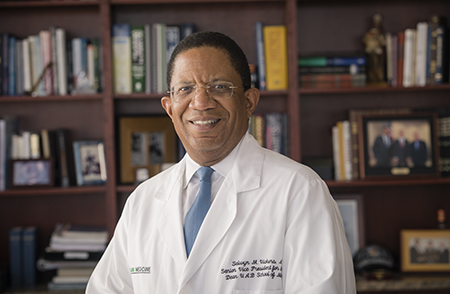
Selwyn M. Vickers, M.D., FACS (Lead Author)
Senior Vice President for Medicine and Dean, UAB School of Medicine
University of Alabama at Birmingham
L.D. Britt, M.D., MPH
Chair, Department of Surgery, Eastern Virginia Medical School
Past President, American College of Surgeons
Deborah V. Deas, M.D., MPH
Vice Chancellor of Health Affairs
Pam and Mark Rubin Dean
University of California Riverside School of Medicine
Henri R. Ford, M.D., MHA
Dean, University of Miami Miller School of Medicine
James E.K. Hildreth, Ph.D., M.D.
President and Chief Executive Officer, Meharry Medical College
Danny O. Jacobs, M.D., MPH, FACS
President, Oregon Health and Science University
Robert L. Johnson, M.D., FAAP
Dean, Rutgers New Jersey Medical School
Interim Dean, Rutgers Robert Wood Johnson Medical School
Talmadge E. King Jr., M.D.
Dean, University of California San Francisco (UCSF) School of Medicine
Ted W. Love, M.D.
President and Chief Executive Officer, Global Blood Therapeutics
Charles P. Mouton, M.D., M.S.
Executive Vice President, Provost, and Dean
The University of Texas Medical Branch School of Medicine
E. Albert Reece, M.D., Ph.D., MBA
Executive Vice President for Medical Affairs, University of Maryland, Baltimore
Dean, University of Maryland School of Medicine
Valeria Montgomery Rice, M.D., FACOG
President and Dean, Morehouse School of Medicine
Joseph A. Tyndall, M.D., MPH
Professor and Interim Dean
University of Florida College of Medicine
David S. Wilkes, M.D.
Dean, University of Virginia School of Medicine
