A new guideline developed by evidence gathered from randomized clinical trials for the management of high blood pressure contains nine recommendations and a treatment algorithm to help doctors treat patients with hypertension. The guideline was published online today by the Journal of the American Medical Association with the goal of providing health care providers with recommendations for the pharmacologic management of hypertension.
A panel appointed to the Eighth Joint National Committee (JNC 8), co-chaired by Suzanne Oparil, M.D., University of Alabama at Birmingham professor of Medicine and director of the vascular biology and hypertensive program in UAB’s School of Medicine, used rigorous evidence-based methods to develop recommendations for blood pressure treatment based on a systemic review of the literature. The report, titled “2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults,” was developed in an effort to assure patients that blood pressure treatment will reduce their disease burden and to give clinicians guidance on hypertension management using the best scientific evidence.
“Hypertension is the most common condition seen in primary care and leads to heart attack, stroke, kidney failure and death if not detected early and treated appropriately,” Oparil said. “This report takes a rigorous, evidence-based approach to recommend treatment thresholds, goals and medications in the management of hypertension in adults. In utilizing randomized clinical trials, we used the highest level of medical evidence that one can have, and this is a process that is endorsed by The Institute of Medicine of the National Academy of Sciences.”
The guideline addresses three questions related to high blood pressure management:
-
In adults with hypertension, does initiating antihypertensive pharmacologic therapy at specific blood pressure thresholds improve health outcomes?
-
In adults with hypertension, does treatment with antihypertensive pharmacologic therapy to a specified blood pressure goal lead to improvements in health outcomes?
-
In adults with hypertension, do various antihypertensive drugs or drug classes differ in comparative benefits and harms on specific health outcomes?
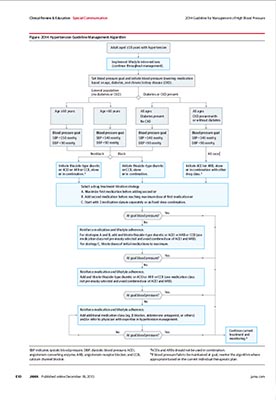 The nine recommendations in the guideline address those three questions.
The nine recommendations in the guideline address those three questions.
Oparil says there are important differences from the past versions of the guideline. The new guideline, for example, focused on the three critical questions above, reviewed pertinent evidence from randomized clinical trials with important clinical outcomes, and used the evidence to develop easily understandable clinical recommendations. The guideline also sought to establish similar treatment goals for all hypertensive populations, except when evidence supports different goals for a particular subpopulation.
Also, rather than defining hypertension or prehypertension, the panel addressed threshold blood pressure levels for starting treatment.
“There is very clear evidence that treating high blood pressure in people 60 and older to a goal of <150/<90 reduces stroke, heart attacks and heart disease,” Oparil said. “There is no evidence that lowering blood pressure further offers additional health benefits, and, further, taking unnecessary medication may increase the burdens on patients, resulting in additional time in the doctor’s office and expensive testing.”
The panel recommended that the blood pressure goal for people under age 60 should be <140/<90, based on expert opinion.
The report also addresses the treatment of blood pressure in those with kidney disease or diabetes. The panel adopted the blood pressure goal of <140/<90 for those groups, based on expert opinion.
Oparil says the panel also recommends that clinicians regularly assess blood pressure, encourage evidence-based lifestyle and adherence interventions, and adjust treatment until goal blood pressure is attained and maintained.
“The potential benefits of a healthy diet, weight control and regular exercise for all persons with hypertension cannot be overemphasized,” Oparil said. “These lifestyle treatments have the potential to improve blood pressure and even reduce medication needs.”
When medication is needed to treat patients, the panel says those with the highest benefit based on the clinical trial evidence are diuretics, calcium channel blockers (CCBs), angiotensin converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs).
“All of those have shown to be useful in the general patient with high blood pressure,” Oparil said. “For nonblack patients, all of those classes seem to be equal. For blacks, CCBs and thiazide-type diuretics seem to be better than the ARBs or ACEIs in first-line treatment. Once that’s been accomplished, add drugs from other classes with complementary mechanisms of action.”
Oparil adds that ACE inhibitors and ARBs should not be used together. They have the same general mechanism of action, give no added benefit when combined and may have adverse effects when used together. Beta blockers are second-tier options.
For a complete look at the panel’s report and further details, visit jnc8.jamanetwork.com/.