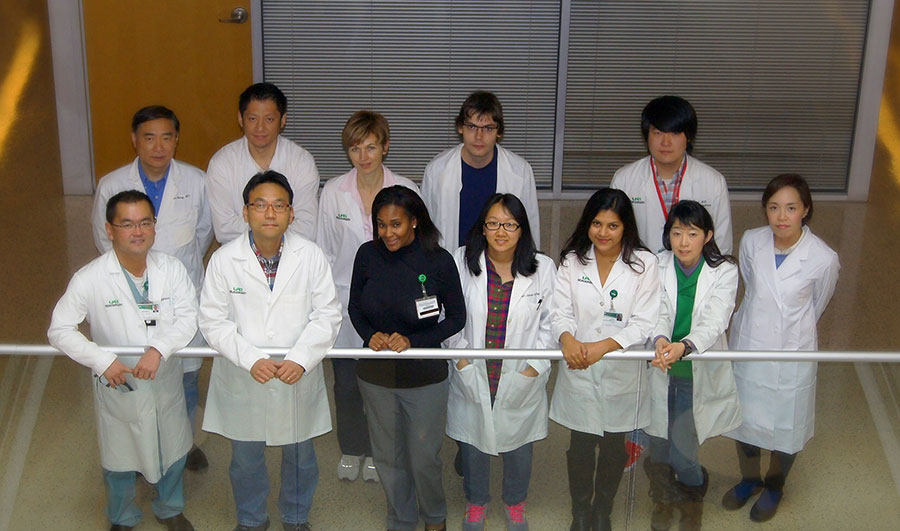
 Front row, from left: Ichiro Nakano, Sunghak Kim, Terry Hamby, Tesha Sherpa, Mutsuko Minata, Shinobu Yamaguchi; Back row: Jun Wan, Zhuo Zhang, Svetlana Komarova, Marat Pavliukov, Jia Wang
Front row, from left: Ichiro Nakano, Sunghak Kim, Terry Hamby, Tesha Sherpa, Mutsuko Minata, Shinobu Yamaguchi; Back row: Jun Wan, Zhuo Zhang, Svetlana Komarova, Marat Pavliukov, Jia Wang
A team of physicians and scientists at the University of Alabama at Birmingham discovered that a kinase protein, mixed lineage kinase 4, also known as MLK4, plays a crucial role in survival of patient-derived brain cancer stem cells in pre-clinical animal models. The findings suggest that MLK4 could potentially be a useful target for cancer treatment.
Protein kinases are key regulators of cell function that constitute one of the largest and most functionally diverse gene families. Until recently, MLK4 was considered a poorly characterized kinase. The UAB team, however, identified this gene from a stepwise screening of molecules that are elevated in cancer stem cells isolated from brain cancer patients.
The findings, published this week online in Cancer Cell, nailed down the novel molecular mechanisms for which MLK4 is essential in cancer stem cells and not in normal cells in the human body. Most importantly, brain cancer patients with higher MLK4 expression have shorter survival despite the current intensive therapies including surgery, chemotherapy and radiotherapy. Nonetheless, there are no MLK4-targeting therapies or clinical trials currently available for patients.
“There is no doubt that society desperately needs new and effective therapies for this life-threatening brain disease. Improvement of patient survival for the past 50 years has been counted by months and not years,” said Ichiro Nakano, M.D., Ph.D., professor in the UAB Department of Neurosurgery and principal investigator of the study. “We, as an international collaborative team centered at UAB, focus on cancer stem cells as a therapeutic target in brain cancers.”
| “There is no doubt that society desperately needs new and effective therapies for this life-threatening brain disease. Improvement of patient survival for the past 50 years has been counted by months and not years. We, as an international collaborative team centered at UAB, focus on cancer stem cells as a therapeutic target in brain cancers.” |
In early 2000, Nakano was involved in a team that isolated cancer stem cells from brain cancers at the University of California at Los Angeles. This discovery gained attention from physicians and scientists because accumulating evidence suggested that cancer stem cells are relatively therapy-resistant and appear to contribute to re-generation of recurrent tumors that subsequently kill affected patients.
“Cancer stem cells share many of the properties of normal stem cells but have also gained transformed cancerous phenotypes,” said Sunghak Kim, Ph.D., an instructor in the UAB Department of Neurosurgery who has led much of the research. “We have been trying to identify the cancer stem cell-specific Achilles heel that could make all the difference.”
While conducting this study, the investigators also found that MLK4-high tumors appear to have Mesenchymal signature, considered to be one process cancers use to become aggressive and therapy-resistant.
“Approximately 35 to 40 percent of glioblastoma patients appear to have Mesenchymal signature. It is also interesting that some non-Mesenchymal cancers seem to shift their phenotype to a Mesenchymal one after therapeutic failure,” Kim said. “We are still collecting more data on this additional piece of information to prove that this is a universal event in brain cancers.”
It is important to note that MLK4 is not expressed in all brain cancers. But now that research indicates that MLK4 is elevated in a subset of brain cancer patients and plays a key role in brain cancer stem cell growth, the next step is to identify targeted therapies that affect the MLK4 in the cancer stem cells.
“We have begun to collaborate with Southern Research Institute to screen drug candidates that selectively target MLK4 in brain cancers,” said Nakano, also a senior scientist at the UAB Comprehensive Cancer Center. “Targeting strategies for MLK4 may work for other cancer types, as we already know that MLK4 is highly expressed in some other malignant types of cancers.”
Nakano added, “Ultimately, we want better outcomes for patients with brain cancer. There’s no question that this is not an easy battle. But by further understanding the molecular mechanisms and applying new targeted therapeutic strategies including MLK4, we are hoping to provide brain cancer patients with more promising and tailored therapeutic approaches.”
Collaborative participants on this project include M.D. Anderson, Ohio State University, University of Texas, Northwestern University, Cincinnati Hospital Medical Center, and a variety of German and Japanese research departments and institutes.
The work was supported by the American Cancer Society, the Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science and Takeda Science Foundation.