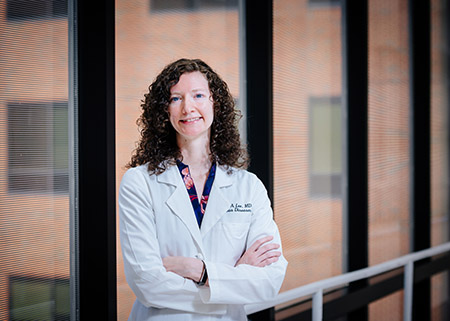
 Infectious diseases physician Rachael Lee, M.D., was the first author of the guidelines.The American College of Physicians has issued recommendations for best practices in the appropriate use of antibiotics for four common conditions, as overuse and antibiotic resistance remain major health care issues. Appropriate Use of Short Course Antibiotics in Common Infections: Best Practice Advice from the American College of Physicians, published today in Annals of Internal Medicine, addresses best practices for prescribing appropriate and short-duration antibiotics for patients presenting with these infections.
Infectious diseases physician Rachael Lee, M.D., was the first author of the guidelines.The American College of Physicians has issued recommendations for best practices in the appropriate use of antibiotics for four common conditions, as overuse and antibiotic resistance remain major health care issues. Appropriate Use of Short Course Antibiotics in Common Infections: Best Practice Advice from the American College of Physicians, published today in Annals of Internal Medicine, addresses best practices for prescribing appropriate and short-duration antibiotics for patients presenting with these infections.
ACP’s Best Practice Advice paper was written by ACP’s Scientific Medical Policy Committee, including first author Rachael Lee, M.D., an assistant professor in the Division of Infectious Diseases at the University of Alabama at Birmingham, and senior author Robert Centor, M.D., professor emeritus in the UAB Department of Medicine.
The paper defines appropriate antibiotic use as prescribing the right antibiotic at the right dose for the right duration for a specific condition. The paper was developed by conducting a narrative literature review of published clinical guidelines, systematic reviews and individual studies that addressed bronchitis with COPD exacerbations, community-acquired pneumonia, urinary tract infections and cellulitis. When clinically safe and supported by evidence, shortening antibiotic duration decreases overall antibiotic exposure, reducing the risk for resistant organisms to develop, as well as lowering a patient’s risk for adverse side effects.
The ACP Best Practice Advice addresses four common conditions that are treated with antibiotics:
COPD and Bronchitis: Clinicians should limit antibiotic treatment duration to five days when managing patients with COPD exacerbations and acute uncomplicated bronchitis who have clinical signs of a bacterial infection (presence of increased sputum purulence in addition to increased dyspnea and/or increased sputum volume).
Community Acquired Pneumonia: Clinicians should prescribe antibiotics for community-acquired pneumonia for a minimum of five days. Extension of therapy after five days of antibiotics should be guided by validated measures of clinical stability, which include resolution of vital sign abnormalities, ability to eat and normal mentation.
 Robert Centor, M.D., professor emeritus in internal medicine, served as senior author of the guidelines.Urinary Tract Infection: In women with uncomplicated bacterial cystitis, clinicians should prescribe short-course antibiotics with either nitrofurantoin for five days, trimethoprim-sulfamethoxazole (TMP-SMZ) for three days, or fosfomycin as a single dose. In men and women with uncomplicated pyelonephritis, clinicians should prescribe short-course therapy either with fluoroquinolones (five to seven days) or trimethoprim-sulfamethoxazole (14 days) based on antibiotic susceptibility.
Robert Centor, M.D., professor emeritus in internal medicine, served as senior author of the guidelines.Urinary Tract Infection: In women with uncomplicated bacterial cystitis, clinicians should prescribe short-course antibiotics with either nitrofurantoin for five days, trimethoprim-sulfamethoxazole (TMP-SMZ) for three days, or fosfomycin as a single dose. In men and women with uncomplicated pyelonephritis, clinicians should prescribe short-course therapy either with fluoroquinolones (five to seven days) or trimethoprim-sulfamethoxazole (14 days) based on antibiotic susceptibility.
Cellulitis: In patients with non-purulent cellulitis, clinicians should use a five- to six-day course of antibiotics active against streptococci, particularly for patients able to self-monitor and who have close follow-up with primary care.
Primary care physicians prescribe antibiotics in 10 percent of all outpatient visits. In 2014, outpatients received over 250 million courses of antibiotics in the United States and at least 30 percent were considered unnecessary and often continued too long. The ACP and the Centers for Disease Control and Prevention have recognized antibiotic-resistant infections as a national threat.
“This guidance on appropriate use of antibiotics is important for practicing physicians when treating these common conditions in our patients,” said ACP president Jacqueline W. Fincher, M.D. “As antibiotic resistance remains a huge issue in the U.S., educating our clinicians to adopt shorter-course antibiotic therapy is paramount.”
ACP’s Best Practice Advice papers address the value of diagnostic tests and therapeutic interventions. They are based on an evaluation of the benefits, harms and cost of a treatment, and how this translates into the value of an intervention.
