Gliomas are brain invaders. The malignant tumor cells branch like tendrils from a central tumor source and spread throughout the brain. Traditional therapies such as surgery can be ineffective if the cells have spread, but University of Alabama at Birmingham researchers may have discovered a way to contain glioma using a drug approved for use in Europe.
 Much the way early explorers of the Old West followed rivers and streams, depending on them to provide drinking water and food, gliomas spread through the brain by following the path of blood vessels, tapping them for the nutrients needed to survive.
Much the way early explorers of the Old West followed rivers and streams, depending on them to provide drinking water and food, gliomas spread through the brain by following the path of blood vessels, tapping them for the nutrients needed to survive.
“An explorer lost in the wilderness without food and water soon succumbs and dies,” said Harald Sontheimer, Ph.D., director of the UAB Center for Glial Biology in Medicine and senior scientist in the UAB Comprehensive Cancer Center. “A glioma that can’t find and tap into a blood vessel also will die.”
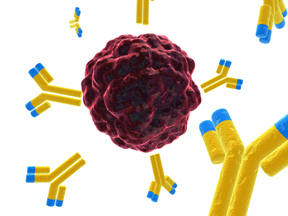
In a paper published March 30, 2011, in the Journal of Neuroscience, Sontheimer and post-doctoral fellow Vedrana Montana, Ph.D., report that glioma cells use bradykinin, a peptide that increases the size of blood vessels, to find blood vessels. Glioma cells carry a receptor called B2R that attracts bradykinin, which navigates the cell to blood vessels. Block the receptor from interacting with bradykinin and the cell will end up lost in the wilderness.
The researchers introduced a B2R-inhibitor known as HOE 140, a laboratory version of Icatibant, a drug approved for use in Europe for treating hereditary angioedema. HOE 140 interfered with the glioma receptor’s opportunity to bind to bradykinin with impressive results.
“We found that 77 percent of glioma cells with bradykinin were able to locate a blood vessel and tap into its nutrients,” said Montana. “However, when we blocked the B2R receptors from interacting with bradykinin, only 19 percent of glioma cells were able to find a blood vessel.”
The researchers used human glioma cells transplanted into a mouse model, and, using time-lapse techniques on a laser-scanning microscope, tracked the ability of the cells to navigate to blood vessels by means of fluorescent markers attached to the cells.
“Targeting the B2R receptors is an elegant and previously unexplored approach to treating gliomas, one of the most devastating types of brain tumor,” said Sontheimer. “Icatibant’s ability to block B2R receptors may prove to be a very promising target for further investigation.”
The American Brain Tumor Association provided funding for this research through a post-doctoral fellowship awarded to Montana.
About 18,000 Americans develop gliomas each year and about half will die within 12 months of diagnosis, according to the Society for Neuroscience.