 From left: Allen and Courtney Harris, Angelynn and mom, Dovie Luckado.
From left: Allen and Courtney Harris, Angelynn and mom, Dovie Luckado.
Dovie Luckado struggles to find the words to explain her unbridled joy and her undeniable pain.
The joy comes from watching her 14-year-old daughter, Angelynn, no longer lying in a hospital bed, no longer struggling to breathe, no longer clinging to life. Angelynn is walking. She is breathing, with a newly transplanted heart and lungs in a rare “heart-lung block” transplant performed at UAB Hospital in November 2015.
But Dovie’s elation comes with the sorrow of knowing the lungs and heart that give Angelynn a new chance at life came at the expense of the grief endured by Allen Harris and Susan and Donald Haynes. The lungs and heart came from Allen’s wife and the Haynes’ daughter — 26-year-old Courtney Harris. Courtney died unexpectedly Nov. 8, 2015, and Angelynn is alive today because Courtney made the decision to be an organ donor when she got her driver’s license more than nine years ago — and because Allen and her parents honored that wish.
“It’s hard because what do you say to them,” Dovie said, her voice cracking as she blinked back tears. “We’re so grateful, and yet that doesn’t seem like enough. A young husband lost his wife of three years. Her parents lost a child, and I got to keep mine because of it. It doesn’t seem right. All we can do is hope that seeing Angelynn do so well gives them some measure of peace.”
Angelynn’s transplant came 113 days after she was first admitted to UAB Hospital because her family had a connection to Courtney’s.
While Angelynn and Courtney never met, Courtney’s extended family knew of Angelynn’s plight. The transplant also happened because of ECMO, a life support technology that kept Angelynn alive while she waited, as well as the daring work and decision-making of UAB School of Medicine physicians who performed a type of transplant on Angelynn that is known to have happened only one other time in the world.
The long walk outside
On Dec. 6, Angelynn Luckado walked out of UAB Hospital, and a video shot by Dovie captured her joy.
“I’m going home,” Angelynn said. “I’m finally going home.”
The journey from hospital to home totaled 149 days. Within that time frame, Angelynn, who was diagnosed with cystic fibrosis at the age of 2, spent 127 days in the Cardiac Intensive Care Unit at UAB; she was on extracorporeal life support — known as ECMO — for 102 days. She spent 21 days under the care of Children’s of Alabama and spent one day in UAB’s Heart and Lung Transplant ICU after she received her rare double-lung and heart transplant. Now, Angelynn is visiting her physicians in The Kirklin Clinic of UAB Hospital one or two days a week instead of being awakened by them every morning.
The determined 14-year-old is indeed finally home.
“We were with the CICU family at UAB beginning the night of July 31 until Dec. 6, and this group of doctors, nurses, perfusionists and respiratory therapists took the best care of Angelynn,” Dovie said. “They saved her so many times and in so many ways. They will always be part of our family.”
“It’s been a hard journey,” Angelynn said. “Two months out of the last four, I couldn’t breathe. I missed the first day of school, the first semester. I didn’t get to experience homecoming. I missed my friends, my home, my sister Rebecca. But when I walked out of the hospital — when I knew I was going home — I knew I was going to be OK. I had been given a second chance, and I was finally free to live that second chance.”
There were many instances during that 149 days when it looked as though that second chance would never occur for Angelynn. Physicians, hospital nurses and staff worked to give Angelynn the best chance at surviving, including employing ECMO, a last-resort technology first developed for use in heart bypass surgery. Physicians have successfully utilized the device as a bridge to heart or lung transplantation. It had to serve as a bridge to both in this instance.
“Angelynn came to the hospital with a cystic fibrosis complication with no thought of a heart-lung transplant,” said Enrique Diaz, M.D., associate professor in the Division of Pulmonary, Allergy and Critical Care Medicine and one of Angelynn’s physicians. “She wound up in bad shape pretty quickly after a planned lung removal, and she was in shock. The family was in shock. The reality is that when she was on ECMO, we talked to her about how a transplant could not be done. They were not expecting the words ‘You’re not going to make it,’ but that was the reality all of us thought she faced.”
UAB physicians have deployed the ECMO technology in a variety ways in the past two years. Doctors have used it to save lives during a flu epidemic, to save the life of a carbon monoxide victim, and even used its Critical Care Transport Service to fly a patient in need of a lung transplant to Birmingham while she was connected to a portable ECMO machine. Angelynn is the first UAB patient to use ECMO as a bridge to a heart and double-lung transplant.
While a heart and double-lung transplant procedure remains a viable therapeutic alternative for patients in specific disease states, the frequency of application has substantially diminished in recent years for several reasons, including a lack of available organs and the tremendous risks involved.
Causes of end-stage cardiopulmonary failure that necessitate heart and lung transplantation range from congenital cardiac disease to idiopathic causes. In Angelynn’s case, it was her cystic fibrosis, a life-threatening, genetic disease that causes persistent lung infections and progressively limits the ability to breathe. The CF precipitated Angelynn’s need, albeit much sooner than normal for most CF patients. Most can make it into their 20s before needing a lung transplant.
The road to transplant
Angelynn had the lower lobe of her right lung removed when she was 6 years old due to cystic fibrosis complications. The lobectomy quickly improved her quality of life, but the family knew then that Angelynn would one day need a lung transplant.
When Angelynn was first admitted to Children’s of Alabama in summer 2015, she had a planned pneumonectomy, or complete removal of the lung. At that point, her left lung was doing the work of both lungs, and the thought was it would be strong enough to carry her into her early 20s when she would then have a lung transplant.
Dovie says Angelynn came through the pneumonectomy wonderfully and did great immediately following the procedure before her remaining left lung suddenly could not clear the carbon dioxide breathed into her body.
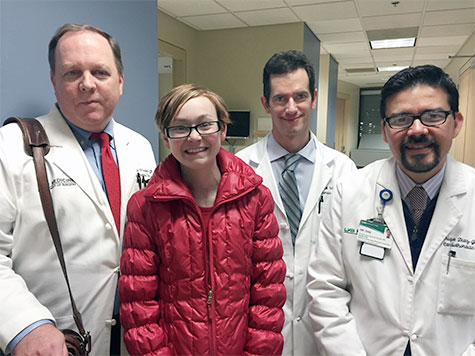 From left: Charles Hoopes, M.D., Angelynn, Keith Wille, M.D., and Enrique Diaz.
From left: Charles Hoopes, M.D., Angelynn, Keith Wille, M.D., and Enrique Diaz.
“She was placed in intensive care and was intubated, and it pretty quickly got to the point where the doctors asked if we wanted her to pass peacefully,” Dovie said. “That just wasn’t an option we wanted to consider. We were evaluated and put on a transplant list in an emergency situation — not what would normally have been a typical CF child’s transplant journey.”
Angelynn was placed on ECMO in UAB Hospital, and for the next 102 days, the machine did all of the breathing for her.
“I literally never saw her chest compress, never saw it move up and down, for the last month prior to her transplant,” Dovie said.
But Angelynn was alive. She was even mobile many days, walking the halls of the Cardiac Intensive Care Unit while hooked to the ECMO machine. On her best days, she would fire Nerf bullets or silly string at her caregivers when they walked into her room — many of whom would return the favor when they had an opportunity. Dovie says those moments kept Angelynn’s spirits up.
There were also days of complete fear for Angelynn and her numerous family and friends who supported her throughout her stay.
She coded twice in the hospital, and had to endure chest compressions in an effort to keep her alive.
One night in late October, Angelynn asked her father, Brandon — a firefighter at the Anniston Army Depot — a question that showed how far her morale had fallen.
“What if I’m not worthy?”
Brandon shared Angelynn’s question with one of her perfusionists, Carl Gagliano, who was taken aback that she would ask such a question. Gagliano was quick to respond, and the impact it made on Angelynn, she says, was significant.
“I remember what Carl told me: ‘If God wanted to take you, He already would have,” Angelynn said. “That kind of rebuilt my hope.”
As a perfusionist, Gagliano is one person on a UAB Hospital team whose sole responsibility is to maintain the ECMO machine and make sure it works properly and provides what the patient needs to stay alive. But as a caregiver, Gagliano and his fellow perfusionists often grow much closer to their patients than just maintaining numbers on a machine. Angelynn was no exception.
When Gagliano heard Angelynn say those words — “What if I’m not worthy? What if I don’t have a purpose?” — it hit him hard.
“Our job is really not motivation, it’s to take care of patients on an ECMO circuit; but I have children, and to see Angelynn lying there … to see her acting like that, it really hit home,” Gagliano said. “I just thought, ‘She’s 14. We’ve got to get her going.’ A lot of times you pray about things, and you just hope for the right words to come out. I guess this time it did.”
Angelynn’s wealth of support
The support Angelynn has received both inside and outside UAB Hospital reaches far and wide. More than 3,100 people have been following her journey on her Prayers for Angelynn Facebook page. The friends and family who visited her while in the hospital were many.
 Angelynn's friends stop by for a visit.Angelynn’s little sister, 13-year-old Rebecca, has been one of her most fervent supporters as well. When Rebecca was not shuffling from family friends’ homes to try to maintain her school obligations, she was by Angelynn’s side. Rebecca missed school only when Angelynn needed her, and she slept in a chair on the weekends so she could spend time with her ailing sister. A stuffed turtle Rebecca gave Angelynn served as her eyes and ears when she could not be there.
Angelynn's friends stop by for a visit.Angelynn’s little sister, 13-year-old Rebecca, has been one of her most fervent supporters as well. When Rebecca was not shuffling from family friends’ homes to try to maintain her school obligations, she was by Angelynn’s side. Rebecca missed school only when Angelynn needed her, and she slept in a chair on the weekends so she could spend time with her ailing sister. A stuffed turtle Rebecca gave Angelynn served as her eyes and ears when she could not be there.
“My sister is my best friend,” Angelynn said. “She’s always there when I need her. She’s the exact opposite of me, so we’re the perfect pair. I don’t think I would have made it through this without her. She was at home, and I knew as soon as I got out of here that I was going back to her. It was a great feeling.”
“Rebecca is a big part of why Angelynn made it through this,” Dovie said. “They have a very special bond. All Rebecca wanted was for Angelynn to get better. Rebecca has never complained about the things she missed out on. I am the most blessed of mothers, and I thank God for my two wonderful daughters.”
Angelynn says her mom, her dad, Brandon, and stepmom, Tara, also have been instrumental in the emotional support they have provided every step of the way.
“I wouldn’t have made it without them either,” Angelynn said. “My mom, Becka, dad and stepmom are the four main people I fought for in all of this. They are who I fought for. I need them, and they need me.”
Dovie says the care provided by the physicians, nurses and staff in the UAB Hospital CICU and other areas was — in her mind — above and beyond what was expected.
“Angelynn’s situation was technically difficult, and her surgery was something that does not happen routinely,” Dovie said. “I know they would say they were just doing their jobs. That might be the case when they performed CPR when her heart stopped. Or when they stood all night and squeezed units of blood into her because the bleeding would not stop. I have lost count of the number of procedures in the OR and at the bedside. But they did more than their jobs. They played with her, laughing while trying to dodge Nerf bullets and silly string. They cheered her up and cheered her on. They made her feel safe. They shed tears for her, both sorrow and joy. They prayed with her and for her. They all did so much more than their jobs.
“And when your doctors text a scared 14-year-old back at 4 a.m., or when they come back in from home because she called their cell, you know you’re in the right place.”
The decision to transplant
Candidates for any type of heart-lung transplantation are generally younger persons with a fatal disease, but the shortage of donor organs combined with a lack of available infrastructure and resources at many medical centers makes this lifesaving procedure unavailable to many individuals. Fortunately, UAB has the infrastructure to make rare transplants like these possible.
Only 19 people received heart-lung transplants from Jan. 1-Sept. 30, 2014, according to the International Society of Heart and Lung Transplantation, and only three of those occurred in children between the ages of 11 and 17.
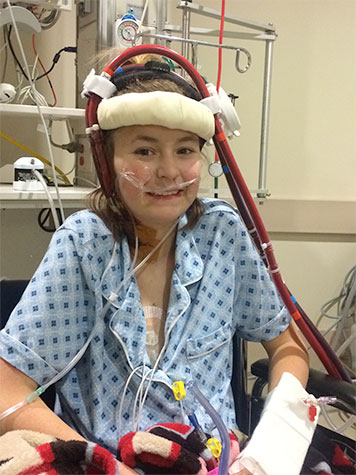 Angelynn spent 121 days on ECMO.The numbers are staggering when it comes to transplant needs and available organs in Alabama. Findings from the Scientific Registry of Transplant Recipients show that only 65 of every 100 Alabamians who die as eligible organ donors are registered through the state. That is below the registry’s recorded national average of 73.6 percent.
Angelynn spent 121 days on ECMO.The numbers are staggering when it comes to transplant needs and available organs in Alabama. Findings from the Scientific Registry of Transplant Recipients show that only 65 of every 100 Alabamians who die as eligible organ donors are registered through the state. That is below the registry’s recorded national average of 73.6 percent.
Demand for organs across the United States also far exceeds the number of people signing up to give, according to data maintained by the United Network for Organ Sharing. There are more than 121,600 people waiting for a lifesaving transplant. On average, 22 people die each day while waiting for a transplant. There were only 12,520 donors from January to October 2015, according to the most recent UNOS data available.
Those were numbers Diaz, Keith Wille, M.D., associate professor of medicine in the Division of Pulmonary, Allergy & Critical Care Medicine, and Charles Hoopes, M.D., chief of the Section of Thoracic Transplantation, have to weigh very critically when determining whether or not a patient should be transplanted.
Hoopes, who joined UAB in 2015, ultimately determined that for Angelynn to survive, she would need what is known as a “block” transplant, or a heart and two lungs from a single donor — a feat that would not be easy given Angelynn’s small size and waning condition. To receive a new heart-lung block, the patient is placed in cardiopulmonary bypass, and the old organs are removed, using caution to ensure that the phrenic nerves are not damaged and that the blood supply to the bronchial arteries is not damaged, to reduce the risk of post-operative bleeding.
The donor heart and lungs are then inserted, and the trachea is sewn into place first. The right atrium is attached next, followed by the aorta. Once the organs are in place, heart-lung bypass stops and blood flow is restored to the heart and lungs. The physician may have to shock the heart to initiate a rhythm, or the heart may start on its own.
Angelynn’s block transplant was necessary for two reasons. First, Angelynn had the pneumonectomy in the summer, which left her without a bronchial stump for Hoopes to sew a single lung into; national survival rates for those who receive single-lung transplants are around 30 percent, so a single-lung donation was not feasible. Second, Angelynn developed severe pulmonary hypertension while awaiting transplant, dropping her heart function to 45 percent. Her heart function fell so much that she was converted from peripheral ECMO cannulation that occurs in the neck to a central cannulation that occurs through the heart. The combination of those events meant she would have to have a new heart in addition to two new lungs.
Hoopes, a surgeon with a particular interest in pediatric pulmonary salvage transplant, says Angelynn’s heart/lung transplant from an ECMO bridge is rare and has been reported in only one other patient after pneumonectomy. It was clear to everyone involved that saving Angelynn would be extremely challenging.
“The only other case I know of was reported from Switzerland five years ago. The general teaching has been if you have a pneumonectomy space, you can’t do much about it; it’s not a transplantable space,” Hoopes said. “In Angelynn’s case, I just thought we could do it technically. I thought it was worth trying given her age; but there’s no doubt it could have gone badly, and no one would have been surprised.”
“The bottom line is that Angelynn was well-cared-for by UAB Hospital nursing, perfusionists and other hospital staff. Dr. Diaz, Dr. Wille, Dr. Jose Tallaj, the medical director of the UAB Heart Transplant Program, and the transplant coordinators have followed Angelynn carefully since her transplant, and the pediatric cardiologists at Children’s of Alabama have gone out of their way to collaborate in the care of her heart. All I had to do was sew in the organs. The rest of it is an act of God.”
Giving the gift of life
Courtney Harris came home from Millington, Tennessee, to Birmingham on Nov. 1. Her husband and high-school sweetheart, Allen, a nine-year Navy veteran stationed in Millington, drove her down that weekend. Courtney came home to spend two weeks with her parents and finalize in-depth plans to open a new business with her mom, Susan Haynes.
Courtney was born as a twin with her brother, Brian, in 1989. They were delivered three months early, and doctors discovered quickly that Courtney had hydrocephalus, a buildup of fluids in the cavities deep within the brain. Her parents were told Courtney would likely never make it home from the hospital, but Courtney entered the world a fighter. She had a shunt placed in her head to relieve the fluid shortly after she was born, and she responded well. Courtney eventually got to go home and had only one other shunt revision in her 26 years; it occurred when she was 18 months old.
“When she was born, we were told she could have numerous medical issues and numerous shunt revisions over the course of her life, if she survived,” said Donald, Courtney’s father. “But she lived a great, healthy life. She had only one shunt revision in 26 years, which is a miracle in and of itself.”
 Courtney and twin Brian
Courtney and twin Brian
On Nov. 6, Courtney began complaining of a headache. Headaches were not uncommon for her, but the intensity she felt this time was more than usual. Donald and Susan took her to a Birmingham hospital the morning of Nov. 7 where she underwent a CT scan. The results looked normal, and Courtney went back home with her parents.
But later that evening, Courtney passed out. She was rushed back to the emergency room and eventually transferred on to UAB. Allen quickly came back to Birmingham from Millington.
The family sat in the hospital waiting to hear news of Courtney’s condition, and as the night went on, the family talked with one another about Courtney’s life and how she packed a lot of good times into her 26 years, and how God had blessed her over those 26 years. As they talked about Courtney, they also talked about how other families weren’t as fortunate with the health of their children as they had been. That’s when Donald’s sister, Rhonda Haynes, mentioned a particular 14-year-old girl who was also in UAB Hospital at that very moment, a young girl who had lived her whole life with cystic fibrosis, was on the transplant list,and was now — like Courtney — fighting for her life.
“We didn’t yet know Angelynn’s name at the time, but we immediately added this young girl my sister mentioned to our prayer list, and we began to pray for both her and Courtney,” Donald Haynes said.
Finally, in the early morning hours of Nov. 8, physicians told Allen and the Hayneses the news they feared. Courtney’s shunt had indeed failed, and her brain showed no activity.
“We were crushed,” Donald Haynes said. “It was a complete shock how quickly it all happened.”
“It was,” said Allen Harris, Courtney’s husband, “the worst news you could ever imagine.”
As the family tried to process the news and the grief, they began thinking about next steps.
Courtney had made the decision to be an organ donor when she got her driver’s license, and Allen and her parents discussed what that meant with the Alabama Organ Center.
“One of the big fears I had when I first thought about it was, ‘Is Courtney going to be presentable when we do a funeral,’” Allen said. “I have to give a lot of credit to the Alabama Organ Center team. They were remarkable. They took us through step by step and made sure we understood everything that would happen and stayed in constant contact with us. It gave us a lot of peace to know that, even though Courtney was donating, it wasn’t going to interfere with actually being able to see her and do an open casket. That’s a fear I think a lot of people have.”
Courtney had an O blood type, which made her a universal donor — meaning she could donate blood to any recipients of any ABO blood group. An AOC donor team member met with Allen later that Sunday afternoon, and while the AOC is bound by law to not give specifics, they told Allen they thought there was someone who might be a match for her organs.
“They said there was this one particular person that they were hoping things would work out for and that she had been on the list for a long time,” Donald Haynes recalled. “Then Allen said, ‘Well, she wouldn’t happen to be 14 years old, would she?’ The person with the Alabama Organ Center almost dropped everything she had. She said, ‘There’s no way you can know that.’ Obviously, she couldn’t tell us, but we knew. We knew.”
Allen, Donald and Susan then asked that this 14-year old girl — they later learned her name, Angelynn —be given any of Courtney’s gifts that she needed, requesting a direct donation.
“It made a huge difference for Angelynn, and it did for us, too,” Donald Haynes said. “We started praying in earnest that Angelynn and the others receiving Courtney’s gifts do well.”
All told, Courtney saved or enriched the lives of six people upon her death, and the number will climb to more than 100 people helped by her soft tissue gifts. As for the six people immediately given a new chance at life upon Courtney’s passing, Allen knows the list by heart.
“Her corneas went to two separate people, one kidney went to an adolescent male, her other kidney and pancreas went to a man in his 40s, her liver went to a man in his 60s, and Angelynn got her heart and lungs,” Allen said. “That’s a list I don’t forget.”
Four days after Courtney passed away and two days after Angelynn’s transplant, Allen came back to UAB Hospital. He had reached out to Dovie through the Prayers for Angelynn Facebook page and introduced himself as Courtney’s husband. Allen said he would love an opportunity to meet Angelynn whenever she and her family felt ready. Dovie told Allen he was welcomed any time he wanted to come by.
“It was Thursday, it was the same day Angelynn walked for the first time after her transplant,” Allen recalled. “It was tough for me to see her, but I knew it was right. And I knew she deserved Courtney’s gifts before I met her. The very first Facebook post I read from Ms. Dovie was a message where she said, ‘I don’t know how to ask someone to give up their loved one or their child so my child can live. As I sit in the hospital right now, I hear helicopters and ambulances coming in, I pray for their families that their loved ones are OK.’ At that point, I knew it was right. I knew Courtney’s heart and lungs went to the right place. And I was proud. And that was really the first big emotion I felt when I saw Angelynn. I felt proud.”
As for Angelynn, she felt grateful. Grateful to Allen, Donald and Susan that they would honor Courtney’s organ donation decision. Grateful that Courtney thought enough of others 10 years ago to decide to be an organ donor.
“Courtney wanted to help someone else and give them a second chance,” Angelynn said. “I appreciate her so much for that. She’s my new guardian angel. I have her heart and her lungs. She lives inside of me, and I need to live my life to the fullest and do the best I can for her and me.”
A way to heal
Just as Dovie Luckado has competing emotions, Allen and the Haynes family do as well. They could not be more thrilled for Angelynn, that she is alive to be with her mom and dad, her sister, her family and friends. But yet Allen misses his wife, and Donald and Susan miss their daughter.
“Courtney was just a beautiful person,” Donald said. “She loved Allen, she loved her family, she loved life. We all couldn’t be more proud of her and the life she lived. And we couldn’t be more proud that she was thinking of someone else when she made the decision to be an organ donor years ago. God knew then what was going to happen, and He was with her, whispering in her ear.”
 From left: Brian Haynes and his wife Claire, Allen Harris, Angelynn, mom Dovie, Susan and Donald Haynes.
From left: Brian Haynes and his wife Claire, Allen Harris, Angelynn, mom Dovie, Susan and Donald Haynes.
Donald Haynes posts messages to his Facebook page every day. It might be a story about Courtney or a remembrance. He is often thanking others for their prayers for his family and for Angelynn and her family. He encourages others who have also lost loved ones too soon.
Allen is heartbroken. He has two pictures on his cellphone. One is a CT image of Courtney’s heart — a photo Allen took when UAB doctors were determining whether her organ would be a fit for Angelynn. The other photo is of two hands he took at Courtney’s bedside in her final moments, his hand interlocked with hers.
But Allen is also thankful and hopeful. He is thankful for the tremendous support he and his in-laws have received from family, friends and the Navy in their time of grief. “Words can’t express how much it means to me, means to us,” he said.
And he is hopeful for Angelynn. He is hopeful that Courtney’s lungs and heart will serve her well for what doctors hope will be at least 15-20 years, until she likely will need another transplant. Allen makes it a point to keep up with Angelynn’s progress from his Tennessee home. He checks Dovie’s posts on Facebook each day, happy to see Angelynn reach each new milestone in her recovery, and proud that Courtney gave a 14-year-old a chance to experience life healthier than she has ever known.
“It’s been emotional,” he said. “We are so happy for Angelynn, and at the same time, sad for our loss. But if it wasn’t for Angelynn, I don’t know how we would have gotten through it. Angelynn has been the light in our day every morning. In the middle of the night, sometimes I will roll over and look at my phone and see what Ms. Dovie has posted about Angelynn and how she’s doing.
“It’s been a way to heal. Angelynn has offered a way for us to heal.”
To be an organ donor upon death and help save the lives of those in need, visit the Alabama Organ Center website and register today. To sign up nationally, visit the U.S. Department of Health & Human Services website.
Learn more about the Division of Cardiovascular Disease’s Heart-Lung Transplant Program here. Information on UAB Medicine’s Transplant Services is available here.