Media contact: Jeff Hansen

If deadlines bother you, working with a cyclotron probably wouldn't be your thing.
Cyclotrons make radioisotopes, radioactive substances that can be incorporated into drugs – radiopharmaceuticals – that are crucial to finding neurological disease, tumors and more with Positron Emission Tomography (PET) scans. But they don't last long.
With most PET radiopharmaceuticals, "you can't make a vial and stick it on the shelf," says Suzanne Lapi, Ph.D., director of the UAB Cyclotron Facility in the UAB Department of Radiology. "You would have nothing left the next morning." The shortest-lived radioisotopes last no longer than an elevator ride – which is why it's so important that UAB's cyclotron and PET scanners are separated by no more than a hallway. PET radiopharmaceuticals are often called "tracers" because only a tiny amount is needed for PET scans.
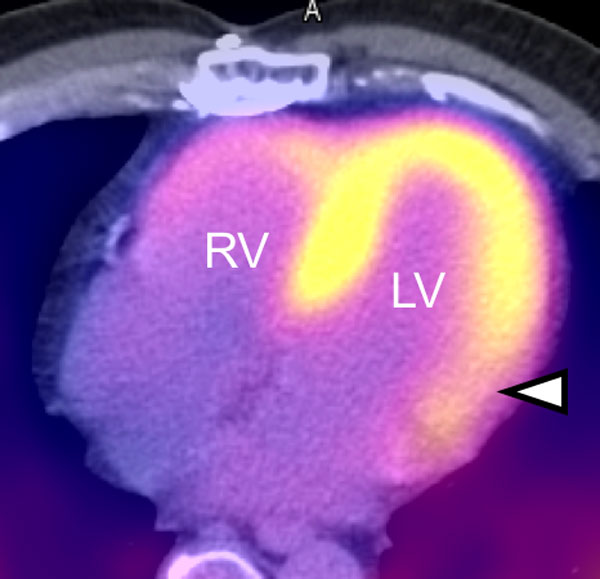 [13N]ammonia-PET/CT measuring blood flow to the heart muscle (myocardial perfusion). The yellow color depicts blood flow measured with ammonia, and the arrowhead shows an area in the left ventricle (LV) of the heart with decreased blood flow due to coronary artery disease. The right ventricle (RV) has a thinner muscle wall and shows less uptake of ammonia.
[13N]ammonia-PET/CT measuring blood flow to the heart muscle (myocardial perfusion). The yellow color depicts blood flow measured with ammonia, and the arrowhead shows an area in the left ventricle (LV) of the heart with decreased blood flow due to coronary artery disease. The right ventricle (RV) has a thinner muscle wall and shows less uptake of ammonia.
Several studies using these short-lived tracers have been carried out already for research in neuroscience, cardiology and cancer at UAB. Many others are in the pipeline for new research using molecular imaging in other fields such as neurology.
For example, over the past several months, Lapi's 60-ton cyclotron has been turning nitrogen gas into precious Carbon-11 to help UAB researchers make tracers that will enable research in Alzheimer's disease like never before. An hour of cyclotron power produces a small amount of Carbon-11. One of the advantages of Carbon-11 and similar radioactive labels is that only a tiny amount of material has to be injected, weighing only a fraction of a grain of salt. But as soon as the cyclotron spins down, the clock is ticking. Within 20 minutes, half of the Carbon-11 will have turned back into nitrogen.
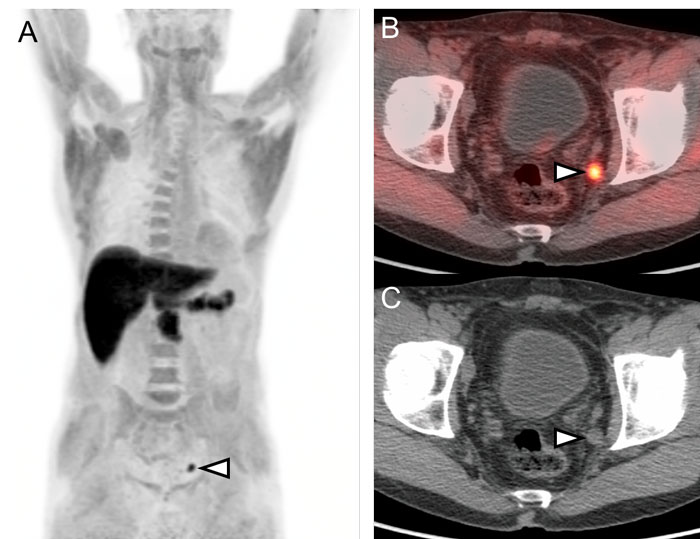 [18F]Fluciclovine-PET/CT in a patient with recurrent prostate cancer. [18F]Fluciclovine is a non-natural amino acid that has increased uptake in prostate cancer. A lymph node involved by prostate cancer is marked with an arrowhead. This lymph node metastasis is seen as a dark spot on the whole body PET image (A) and a white/orange spot on the PET/CT image (B). The lymph node can be seen on the CT image (C), but the uptake of the PET tracer is key to confirming the presence of prostate cancer in this node.
[18F]Fluciclovine-PET/CT in a patient with recurrent prostate cancer. [18F]Fluciclovine is a non-natural amino acid that has increased uptake in prostate cancer. A lymph node involved by prostate cancer is marked with an arrowhead. This lymph node metastasis is seen as a dark spot on the whole body PET image (A) and a white/orange spot on the PET/CT image (B). The lymph node can be seen on the CT image (C), but the uptake of the PET tracer is key to confirming the presence of prostate cancer in this node.
Before they can disappear, chemists attach the radioactive Carbon-11 molecules to a substance known as Pittsburgh compound B (PiB). When human studies begin, the technicians will then fill a syringe with the compound and pass it through a special drawer to the facility's radiopharmacy, where the final dose will be prepared for the waiting patient. Within a few minutes, the patient's circulatory system will carry the radiopharmaceutical PiB into the brain, where it can congregate around abnormal clumps of protein called beta-amyloid plaques. After the injection, a PET/MRI scanner will capture images unlike any ever taken in Alabama – a living brain under siege from Alzheimer's.
"An exciting time"
"This is really the first time we're able to get a window on the molecular changes going on in Alzheimer's," says Erik Roberson, M.D., Ph.D., associate professor of neurology and neurobiology in the UAB School of Medicine, Patsy W. and Charles A. Collat Professor of Neuroscience, and director of the UAB Alzheimer's Disease Center. With PET imaging and PiB, Roberson will be able to see beta-amyloid protein plaques scattered about the brains of his patients. Some beta-amyloid PET studies have been performed at UAB with tracers produced elsewhere, as shown in the image below. However, PiB production at UAB will be critical to meeting the research needs of the UAB Alzheimer's Disease Center.
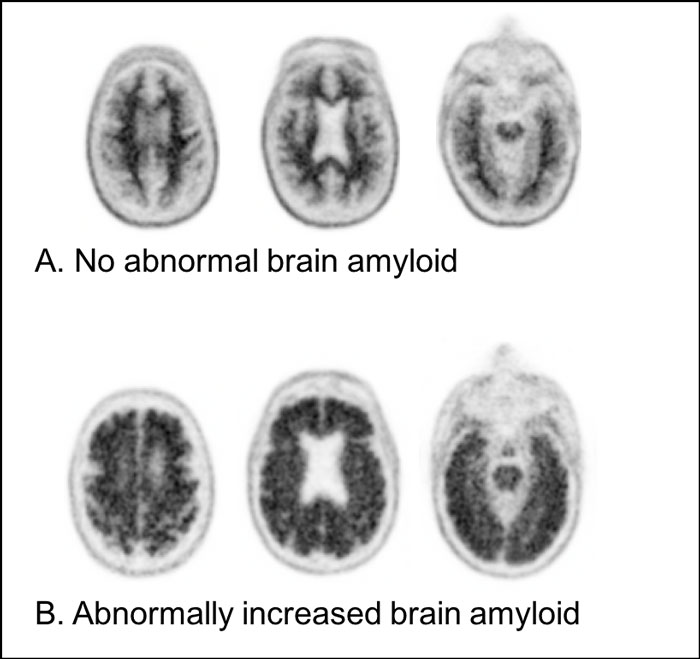 Brain amyloid PET images from two different patients with cognitive impairment including memory problems. The top row shows images from an [18F]florbetapir brain PET study in a patient without abnormally increased amyloid in the brain. The dark areas are due to higher amounts of the amyloid PET tracer in the white matter of the brain than the cortex, which is along the surface of the brain. The lack of increased amyloid indicates that it is very unlikely that this patient’s cognitive impairment is due to Alzheimer’s disease. The bottom row shows [18F]florbetapir brain PET images in a patient with abnormally increased amyloid in the brain. In this patient, the cortex along the surface of the brain is seen as dark due to increased amyloid PET tracer binding, indicating the presence of amyloid, which can occur in Alzheimer’s disease.
Brain amyloid PET images from two different patients with cognitive impairment including memory problems. The top row shows images from an [18F]florbetapir brain PET study in a patient without abnormally increased amyloid in the brain. The dark areas are due to higher amounts of the amyloid PET tracer in the white matter of the brain than the cortex, which is along the surface of the brain. The lack of increased amyloid indicates that it is very unlikely that this patient’s cognitive impairment is due to Alzheimer’s disease. The bottom row shows [18F]florbetapir brain PET images in a patient with abnormally increased amyloid in the brain. In this patient, the cortex along the surface of the brain is seen as dark due to increased amyloid PET tracer binding, indicating the presence of amyloid, which can occur in Alzheimer’s disease.
It's easy to spot Alzheimer's post-mortem, when pathologists look at samples of brain tissue and find the hallmark beta-amyloid plaques and tangles of tau proteins that mark the disease. "In the clinic, we use memory problems that worsen over time as a proxy," Roberson says. But it's not the same thing, he notes. Does a patient really have Alzheimer's, or is it another form of dementia? How is the patient's brain responding to treatment? With PET imaging, doctors can now answer these questions. "It's an exciting time in Alzheimer's research," says Roberson. That is, if you have the expensive, highly complex machinery to create the specialized particles that make PET run.
Heavy duty
In 2013, a crane lowered UAB's cyclotron into its concrete- and steel-lined vault in the Comprehensive Cancer Center's Wallace Tumor Institute building on 6th Avenue. PET imaging is growing ever more useful as a tool for treating and studying cancer, neurological diseases, heart disease and more. And to be a leader in PET research, it helps to have your own cyclotron.
 UAB Cyclotron Facility director Suzanne Lapi, Ph.D., and senior biomedical engineering student Retta El-Sayed entering the cyclotron vault. Discover El-Sayed's cyclotron journey in "Force for Good."
UAB Cyclotron Facility director Suzanne Lapi, Ph.D., and senior biomedical engineering student Retta El-Sayed entering the cyclotron vault. Discover El-Sayed's cyclotron journey in "Force for Good."
UAB's 24 megaelectronvolt (MeV) model is a high-power, high-current machine capable of accelerating particles to more than 1/16th the speed of light. All that power and speed is used to induce nuclear reactions on common elements such as oxygen and nitrogen. The cyclotron can bombard the nucleus of an Oxygen-18 atom with a proton and eject a neutron, transforming it into a completely different element: fluorine. When the radioactive Fluorine-18 decays, a positron is emitted, which collides with electrons to produce gamma rays that are detected by the PET scanner. The Fluorine-18 can also be chemically conjugated – tagged – to interesting substances, like glucose, or a new drug, so that researchers and clinicians can track exactly where they go in the body. For example, Fluorine-18 can be incorporated into a tracer called FLT which is an analogue for the DNA (deoxyribonucleic acid) building block thymidine and can be used to image tumor growth.
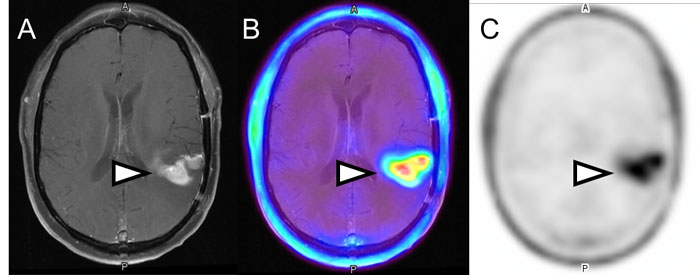 Fused PET and MRI images in a patient with glioblastoma, a very aggressive form of brain cancer. The tracer [18F]FLT, a thymidine analogue, is being used to measure the rate of proliferation (cell division) of the tumor. The brain tumor is marked with a white arrow on the contrast-enhanced MR images (A), the fused [18F]FLT-PET and MR images (B), and the [18F]FLT-PET only images (C).
Fused PET and MRI images in a patient with glioblastoma, a very aggressive form of brain cancer. The tracer [18F]FLT, a thymidine analogue, is being used to measure the rate of proliferation (cell division) of the tumor. The brain tumor is marked with a white arrow on the contrast-enhanced MR images (A), the fused [18F]FLT-PET and MR images (B), and the [18F]FLT-PET only images (C).
"We're here to provide service and new tools for the great research at UAB," says Lapi. The cyclotron is just across the hall from the PET/CT scanners of the UAB Advanced Imaging Facility, notes AIF director Jonathan McConathy, M.D., Ph.D., who is also division director for Molecular Imaging and Therapeutics in the radiology department. "For some tracers that doesn't make a big difference," he says. But for really short-lived tracers, such as Oxygen-15, with a two-minute half-life, "we can have the Cyclotron Facility make that and then immediately use it in the Advanced Imaging Facility," McConathy says.
The AIF has two PET/CT systems, as well as a PET/MR system – "a new technology that allows PET and MRI acquisition at the same time," McConathy says. "We're one of the few in the Southeast that has such a system, which we can use for clinical work and for research."
Gone in 60 seconds – or less
The time it takes for a tracer to turn back into its original form varies, from days to seconds. Every day, Lapi's team works to make the tracers that UAB researchers and clinicians will need for PET imaging studies, including Carbon 11-labeled PiB (half-life 20 minutes) for studying Alzheimer's; Zirconium-89-labeled trastuzumab (half-life 78 hours) for examining the presence of the HER2 protein on breast tumors; Fluorine-18 (half-life 110 minutes) for imaging amino acid transport in brain tumors with fluoroethyl tyrosine (FET); and Nitrogen-13-labeled ammonia (half-life 10 minutes) for measuring cardiac blood flow.
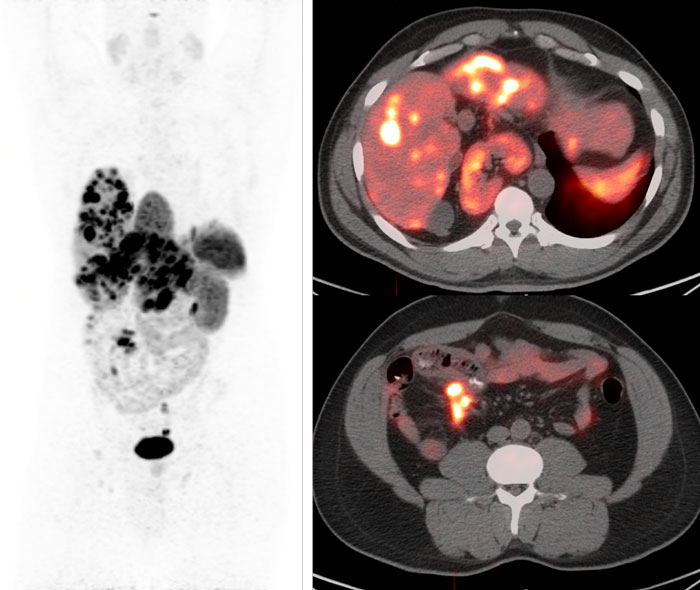 [68Ga]DOTATATE-PET/CT in a patient with a neuroendocrine tumor that has spread to the liver. Areas involved by tumor are marked with arrowheads. The whole-body PET image (A) shows [68Ga]DOTATATE binding to neuroendocrine tumor as dark spots, while the fused PET/CT images of the liver (B) and the lower abdomen (C) show binding as white and orange spots.
[68Ga]DOTATATE-PET/CT in a patient with a neuroendocrine tumor that has spread to the liver. Areas involved by tumor are marked with arrowheads. The whole-body PET image (A) shows [68Ga]DOTATATE binding to neuroendocrine tumor as dark spots, while the fused PET/CT images of the liver (B) and the lower abdomen (C) show binding as white and orange spots.
As Lapi's team synthesizes additional tracers for research and clinical use, more patients at UAB are now receiving PET imaging as part of their care. This summer, the group began producing Gallium-68-DOTATATE, an FDA-approved compound that is used to help determine the best treatment for neuroendocrine tumors. "We're the only place in Alabama" able to offer Gallium-68-DOTATATE imaging, Lapi says. Since this option became available in June 2017, dozens of patients have been scanned.
The advantage of PET tracers' short half-lives, says Lapi, is that "patients won't be radioactive the next day." Of course, "radioactive" can be an unsettling word, especially in connection with cancer. But it should be put in context, says McConathy, a radiologist and nuclear medicine physician, who is one of the physicians on duty whenever patients receive radiopharmaceuticals. PET studies involve the same radiation a person would get from other types of diagnostic imaging studies, like CT, he notes.
New era for Alzheimer's research
Unlike CT, or MRI or X-rays, PET reveals active processes going on in the body. With PET scans using PiB as a tracer, "you can look at the overall pattern of where amyloid-beta is in the brain, and at what levels," Roberson says.
At the moment, this information doesn't directly affect treatment for Alzheimer's. Because the limited therapies currently available don't actually target the amyloid and are effective in other dementia syndromes, "we'll often use them whether a scan is positive or not," Roberson says. That's the reason that the federal Centers for Medicare and Medicaid Services has so far declined to cover PET testing for amyloid beta, despite FDA approval in 2012. But new drugs in the research pipeline could change all that. One is Biogen's aducanamab, which made a big splash with phase 2 trial results in Nature in 2016. If these drugs make it to market, they will be expensive, and tests to identify appropriate patients will suddenly be very desirable. PET scans in Alzheimer's "are on the verge of being more useful" in the clinic, Roberson says.
| Support UAB Alzheimer's research |
PET is already proving its value in Alzheimer's research. For the past several years, UAB's Alzheimer's Disease Center has participated in a worldwide trial, known as DIAN, that is enrolling members of families with one of several Alzheimer's-associated mutations in the APP, PSEN1 or PSEN2 genes. "These are people who will get the disease starting in their 40s," much earlier than typical Alzheimer's patients, Roberson says. "And half of their kids will inherit the gene. It's become a really important area of study."
Those telltale mutations let researchers identify people who are very likely to get Alzheimer's – before the disease has taken a toll. "A lot of the trials in Alzheimer's disease have not worked," Roberson says. "We think one reason is we have been doing them in people who have had the disease for quite a while. We think it may be too late to use these treatments by then. So we're trying to treat people earlier, ideally before they have any symptoms. If you see a person who is 25 [with an Alzheimer's-predisposing mutation], and his parent got it at 45, he's roughly t-minus 20 years out. What happens if you treat him then?"
This is the hypothesis that DIAN is testing. Participants receive antibodies against amyloid-beta. Researchers then use PET imaging to see if the drugs have reduced amyloid-beta accumulation. "We have already enrolled people in DIAN, but we had to send them to St. Louis for imaging," Roberson says. Now, participants will be able to stay close to home.
UAB's Alzheimer's Disease Center is getting ready to launch another study, which will use PET scans as well as memory tests, medical history, blood draws and more, to investigate the disparities in Alzheimer's diagnoses in the Deep South. "There is a higher risk of Alzheimer's disease in African Americans," Roberson explains. "There is also a higher risk in people with vascular issues, like diabetes, heart disease and obesity." This study will gather clues as to why that is the case.
"In this day and age, it's almost impossible to be a cutting-edge Alzheimer's disease center without a cyclotron and PET imaging," Roberson says.
Exploring new boundaries
McConathy and Lapi are each working to develop new PET tracers.
"They could help us understand the underlying biological process of a disease, or guide drug development by revealing if a drug is reaching its target, or speed up clinical trials by selecting the right person to be in the clinical trial," McConathy says.
For several years, McConathy has been interested in amino acids, the building blocks of proteins. "It turns out that many cancers take up more amino acids than normal tissues," he says. The amino acids enter cells through different transporter proteins. "One of our strategies is to try to target several transporters," McConathy says. Working with two postdoctoral chemists, he has developed several amino acid tracers that are effective in lab tests and could eventually be used in human trials. Amino acid tracers could be used "to learn something important about a tumor, or potentially guide treatment," he says.
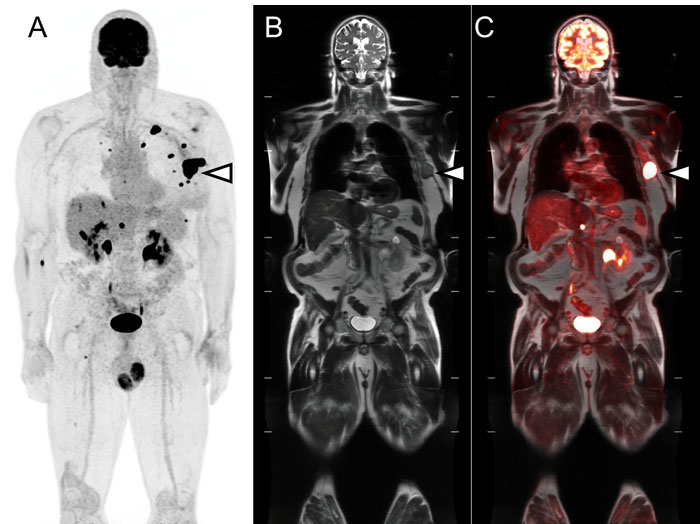 [18F]FDG-PET/MRI in a patient with melanoma that has spread throughout the body. Areas of FDG uptake by melanoma are seen as dark spots on the whole-body image (A). An arrowhead marks a large metastasis in the left chest wall which can be seen on the whole body MR image (B) and on the fused PET/MR image (C).
[18F]FDG-PET/MRI in a patient with melanoma that has spread throughout the body. Areas of FDG uptake by melanoma are seen as dark spots on the whole-body image (A). An arrowhead marks a large metastasis in the left chest wall which can be seen on the whole body MR image (B) and on the fused PET/MR image (C).
The researchers also study new tracers developed elsewhere. McConathy and his colleagues hope to begin small human studies of the tracer fluoroethyl tyrosine, known as FET, which is used for brain tumor imaging. "There's fairly good evidence that it does better than MRI alone," McConathy says. "MRI has trouble sometimes in determining tumor boundaries. It can be hard to tell if a tumor is growing, or if you are seeing the effects of treatment. We think tracers like FET could help."
"We're working on a radiopharmaceutical for looking at HER2 protein expression in breast cancer," Lapi adds. "Many patients get HER2 therapy; the idea is to develop imaging agents that would be able to tell a patient's status without taking a biopsy." PET is an important tool in the development of precision medicine, Lapi notes. "Long-term, we could use molecular imaging to help select who should get what type of therapy. If we know your tumor is expressing certain receptors, we know how to target it for effective treatment."