University of Alabama at Birmingham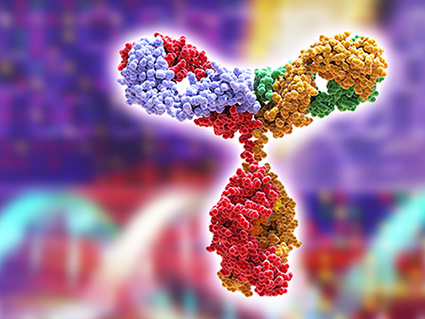 researchers have added fresh evidence that early exposure to vaccine-, bacterial- or microbiota-derived antigens has a dramatic effect on the diversity of antibodies an adult mammal will have to fight future infections by pathogens. This antibody diversity is called the clonal repertoire — basically different single cells with distinct antibody potential that can multiply into a large clone of cells, all producing that distinct antibody.
researchers have added fresh evidence that early exposure to vaccine-, bacterial- or microbiota-derived antigens has a dramatic effect on the diversity of antibodies an adult mammal will have to fight future infections by pathogens. This antibody diversity is called the clonal repertoire — basically different single cells with distinct antibody potential that can multiply into a large clone of cells, all producing that distinct antibody.
In a mouse study published in the journal Immunity, they looked at a group of immune cells called B-1 B cells. Although all B cells have the ability to develop into antibody-secreting cells to control pathogens, innate-like B-1 B cells originate from a developmental program that is distinct from conventional B cells.
The UAB researchers, led by first author J. Stewart New, Ph.D., and co-senior authors John Kearney, Ph.D., and R. Glenn King, Ph.D., UAB Department of Microbiology, looked at a subset of B-1 B cells that react to N-acetyl-D-glucosamine-containing Lancefield Group A carbohydrate, or GAC, a cell wall polysaccharide of the bacterial pathogen Streptococcus pyogenes.
They asked the question, how much will clonal diversity differ in mice grown under sterile germ-free conditions, versus mice with a normal gut microbiota from birth, or mice with a normal microbiota that are also vaccinated as neonates with GAC-bearing S. pyogenes. To answer, they sequenced the immunoglobulin heavy chain variable region, or IGHV region, for single B cells labeled with GAC. Single-cell sequencing has exploded in the past decade as a powerful research tool that takes biology to a new depth of understanding.
New, Kearney, King and colleagues found that environmental antigen-dependent selection events play a significant role to shape the GAC-reactive B-1 B cell clonal repertoire. New is a postdoctoral fellow, Kearney is a professor, and King is assistant professor of microbiology in the UAB School of Medicine.
In general, germ-free mice had a low IGHV clonal diversity, while both conventional mice and neonatal-vaccination mice had high clonal diversities. However, the conventional and neonatal-vaccination mice differed. Both showed that the establishment of IGHV region 6-3 GAC-reactive B cell clonal dominance was microbiota-dependent; but in addition, the neonatal immunization with S. pyogenes expanded the typically minor IGHV region 7-3 GAC-reactive clonotypes, compared to those clonotypes in the conventional mice.
The researchers found that colonization of adult germ-free mice promoted N-acetyl-D-glucosamine-reactive B-1 B cell development and led to clonally related immunoglobulin A-positive plasma cells in the small intestine. Plasma cells differentiate from B cells, and they are the ones that produce antibody. Immunoglobulin A secretion in the gut is beneficial because it helps constrain the composition and inflammatory activity of the normal microbiota in the small intestine.
Kearney says that understanding how exposure to microbial antigens in early life determines the clonality and ensuing antibody responses of the B-1 B cell repertoire has implications for vaccination approaches and schedules.
B-1 B cells also are known to produce natural immunoglobulin M. Deficiencies of immunoglobulin M have been associated with increased rates of autoimmunity and allergic diseases. The dramatic effect of early exposure to vaccine or bacteria for clonal diversity seen in the current research, Kearney said, “may provide an alternative mechanistic explanation for the influence of environmental antigens on the allergic and autoimmune disease susceptibility, which is often discussed in context of the hygiene hypothesis.”
The hygiene hypothesis suggests that a reduction in infections in Western countries — due to better hygiene — has led to an increase in autoimmune and allergic diseases.
Co-authors with New, Kearney and King of the study, “Neonatal exposure to commensal-bacteria-derived antigens directs polysaccharide-specific B-1 B cell repertoire development,” are Brian L.P. Dizon and Alexander F. Rosenberg, UAB Department of Microbiology; and Christopher Fucile, UAB Informatics Institute.
Support came from National Institutes of Health grants AI14782, AI100005, AI120500, A1007051, DK082277 and GM008861.
At UAB, Kearney holds the Endowed Professorship in Immunology in the Department of Microbiology.
