 Kevin Harrod, Ph.D.Jeanne Marrazzo, M.D., director of Infectious Diseases, got a text at the end of Wednesday’s four-hour School of Medicine COVID-19 Research Symposium that highlighted the broad and breakneck work done at the University of Alabama at Birmingham since March 2020.
Kevin Harrod, Ph.D.Jeanne Marrazzo, M.D., director of Infectious Diseases, got a text at the end of Wednesday’s four-hour School of Medicine COVID-19 Research Symposium that highlighted the broad and breakneck work done at the University of Alabama at Birmingham since March 2020.
“It seems like we’ve done 10 years of work in seven months!” she told participants.
Presentations by eight leading UAB researchers buoyed that sentiment. Among the work:
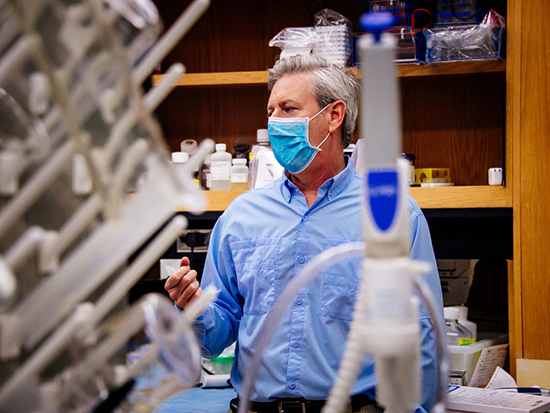
- Kevin Harrod, Ph.D., described how his team used computers and artificial intelligence to identify 145 existing drugs that might have potential to treat SARS-CoV-2, the COVID-19 virus, and then tested them against live virus to identify 11 that reduced 90 percent of viral growth in cell cultures.
- Sixto Leal, M.D., Ph.D., director of the Clinical Microbiology, Fungal Reference Laboratory, told how his team created its own COVID-19 PCR test in early March when none was available nationally, and how the test performed better than all others created elsewhere in a later, nationwide comparison. This test allowed UAB hospitals and regional hospitals in Alabama to reopen for regular care, and from March 17 to this August, his team was able to increase the rate of COVID-19 testing from 150 tests a day to more than 11,300 tests a day.
- Nathan Erdmann, M.D., Ph.D., spoke of how his team — with extraordinary supporting efforts from hospital, research and clinical staff — was able to enroll UAB patients in national COVID-19 trials, including the successful remdesivir trial. “Everything is harder” in clinical trials with a potentially deadly virus, he said. Clinicians had to mitigate their exposure to infection, while being careful not to use up too much of the personal protective equipment that was scarce earlier this year. Talking to very ill participants was much harder, as was staying safe while collecting samples of blood and saliva, and then processing those samples.
One hallmark of all eight presentations? An extreme interdisciplinary collaboration of researchers and clinicians across the hospital and university campus, that co-convener Etty “Tika” Benveniste, Ph.D., called “remarkable.” Research presented by Fran Lund, Ph.D., for example, involved eight different labs and 30 researchers.
Here are brief highlights of each presentation.
The first two presenters, Lund and Paul Goepfert, M.D., looked at how two kinds of the immune system’s white blood cells respond in patients with COVID-19.
Lund, an international expert in B cell biology, was able to isolate B cells from patients that made antibodies against the SARS-CoV-2 virus spike protein. Her team found that many of these antibodies were cross-reactive against the spike proteins from SARS or MERS, which suggested that the antibody protection might wane. She also briefly mentioned her work to test the Altimmune Inc. intranasal vaccine candidate that would be the first intranasal vaccine for COVID-19 and might be effective at preventing transmission.
 Steven Rowe, M.D.Goepfert’s team found a surprising result: Peripheral T follicular helper cells against SARS-CoV-2 continue to increase during convalescence, and they are more activated in severe patients who are in intensive care.
Steven Rowe, M.D.Goepfert’s team found a surprising result: Peripheral T follicular helper cells against SARS-CoV-2 continue to increase during convalescence, and they are more activated in severe patients who are in intensive care.
Immunologic studies like those of Lund and Goepfert are vital for understanding how the body responds to SARS-CoV-2 infection, as a prelude to learning how to better treat the disease.
In the section on optimizing diagnosis and treatment, Erdmann talked about several other clinical trials besides the remdesivir trial. He noted that UAB has been quite successful in minority enrollment for inpatient trials, and said UAB researchers have been able to enroll 159 convalescent patients and 846 hospitalized patients for donations of high-quality biological samples like peripheral blood monocytes, blood plasma, urine and oral saline rinses.
After he finished, Marrazzo said, “You highlighted the absolutely herculean efforts to do this exceptionally collaborative work at UAB.”
Besides the creation and expansion of the UAB COVID-19 test, Leal described how his team was able to adapt that test to screen 250,000 students who were returning to Alabama colleges in August, by using a pooled-sample method. Now, as flu season approaches, the clinical lab is adjusting its test to detect both SARS-CoV-2 and seasonal influenza in a single test. They are also beginning to incorporate prognostic tests of things like interferon-beta or various cytokines into the COVID-19 test. The goal is being able to identify those who are more at risk for severe disease.
In Harrod’s drug screening, he identified tocopherol polyethylene glycol succinate (TPGS) — an existing drug that is a Vitamin E precursor — as a drug that acts in synergy with remdesivir. This is important because the TPGS could then lessen the amount of remdesivir needed to treat patients. Remdesivir is in short supply. Intriguingly, his team also found that ivacaftor, a cystic fibrosis drug, is effective against SARS-CoV-2 in the cell culture assays, opening the door to studying its mechanism of action.
The second presenter in basic science discovery, along with Harrod, was Steven Rowe, M.D., director of the Gregory Fleming James Cystic Fibrosis Research Center at UAB. He is testing ferrets as an animal model of severe COVID-19 disease, to fill the urgent need for such a model. His team has found that infection with SARS-CoV-2 disrupts mucociliary clearance in the ferret trachea, as measured by micro-optical coherence tomography, which is similar to the laser eye test that creates a profile of a patient’s retina. This test is now being adapted to quantify mucociliary clearance — the escalator-like movement of mucus from the lungs to the throat — in patients with COVID-19.
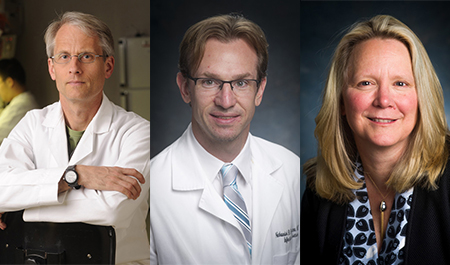 Paul Goepfert, M.D., Nathan Erdmann, M.D., Ph.D., and Fran Lund, Ph.D.The final section of the symposium focused on COVID-19 and health disparities.
Paul Goepfert, M.D., Nathan Erdmann, M.D., Ph.D., and Fran Lund, Ph.D.The final section of the symposium focused on COVID-19 and health disparities.
Mona Fouad, M.D., noted that COVID-19 deaths are higher in African Americans and Hispanics than whites, and she said that, as the pandemic arrived, the UAB Minority Health and Health Disparities team pivoted to COVID-19. They created a Community Mobile Testing Model with three parts: engaging and educating communities about COVID-19 and dispelling myths; bringing mobile testing to vulnerable communities; and creating patient navigators to help people with COVID-19. Navigators are people who have had experiences similar to those of the community’s people and understand their needs.
Jefferson County CARES Act funding expanded the program to 33 test sites in 18 communities in the county. Of the adults tested, Hispanics had a 29 percent positivity rate, African Americans 9 percent and whites 5 percent.
The final UAB presenter was Selwyn Vickers, M.D., dean of the UAB School of Medicine. He said a meeting he had with 13 Black medical leaders nationwide identified COVID-19 as a crisis within a crisis. African Americans already had health disparities, caused in part by disparities in education and socio-economic determinants, before the added burden of a pandemic.
The deadly combination of COVID-19 with the preexisting social determinants was like throwing gasoline on a fire, he said, a combination of smoldering chronic disease and an acute respiratory infection. Even more than African Americans, the worst-hit in the United States are Native Americans.
To help address disparities, Vickers said we need to prepare for a second surge of COVID-19, ensure equitable treatment and vaccine availability, invest in public health, and invest in reducing the social determinants of health disparities.
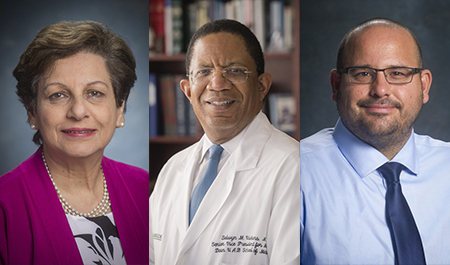 Mona Fouad, M.D., Selwyn Vickers, M.D., and Sixto Leal, M.D., Ph.D.At UAB, Marrazzo is the C. Glenn Cobbs, M.D., Endowed Professor in Infectious Diseases and a professor in the Department of Medicine; Benveniste is the senior vice dean for Basic Sciences in the School of Medicine, the Charlene A. Jones Endowed Chair in Neuroimmunology, and professor, Department of Cell, Developmental and Integrative Biology; Lund is the Charles H. McCauley Professor and chair, Department of Microbiology; Goepfert is director of the Alabama Vaccine Research Clinic and professor, Department of Medicine, Division of Infectious Diseases; and Erdmann is an assistant professor, Department of Medicine, Division of Infectious Diseases.
Mona Fouad, M.D., Selwyn Vickers, M.D., and Sixto Leal, M.D., Ph.D.At UAB, Marrazzo is the C. Glenn Cobbs, M.D., Endowed Professor in Infectious Diseases and a professor in the Department of Medicine; Benveniste is the senior vice dean for Basic Sciences in the School of Medicine, the Charlene A. Jones Endowed Chair in Neuroimmunology, and professor, Department of Cell, Developmental and Integrative Biology; Lund is the Charles H. McCauley Professor and chair, Department of Microbiology; Goepfert is director of the Alabama Vaccine Research Clinic and professor, Department of Medicine, Division of Infectious Diseases; and Erdmann is an assistant professor, Department of Medicine, Division of Infectious Diseases.
Also, Leal is assistant professor, Department of Pathology; Harrod is the Benjamin Monroe Carraway Endowed Chair and professor, Department of Anesthesiology and Perioperative Medicine; Rowe is professor, Department of Medicine, Division of Pulmonary, Allergy and Critical Care Medicine; Fouad is senior associate dean of Diversity and Inclusion, professor, Department of Medicine, and director, Division of Preventive Medicine; and Vickers is the James C. Lee Jr. Endowed Chair, senior vice president for Medicine and dean, School of Medicine.
