 With increasing prevalence of childhood obesity, non-alcoholic fatty liver disease has emerged as the most common cause of liver disease among children and adolescents in industrialized countries.Amy Goss, Ph.D., assistant professor in the University of Alabama at Birmingham’s Department of Nutrition Sciences, has received a $3 million R01 grant to implement a family-based diet intervention to treat fatty liver disease and obesity in adolescents.
With increasing prevalence of childhood obesity, non-alcoholic fatty liver disease has emerged as the most common cause of liver disease among children and adolescents in industrialized countries.Amy Goss, Ph.D., assistant professor in the University of Alabama at Birmingham’s Department of Nutrition Sciences, has received a $3 million R01 grant to implement a family-based diet intervention to treat fatty liver disease and obesity in adolescents.
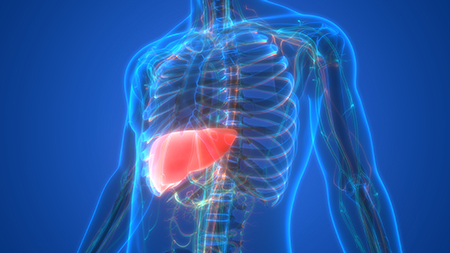
With increasing prevalence of childhood obesity, non-alcoholic fatty liver disease has emerged as the most common cause of liver disease among children and adolescents in industrialized countries. For children and adolescents ages 2 to 19, the prevalence of obesity has reached 17 percent and affects nearly 13 million children in the United States.
Non-alcoholic fatty liver disease refers to a spectrum of liver diseases ranging from simple fat infiltration to non-alcoholic steatohepatitis, or NASH, fibrosis and cirrhosis.
 Amy Goss, Ph.D.
Amy Goss, Ph.D.
(Photo by: Katherine Mullen)It has been reported that approximately 20 percent of patients with NASH will progress to cirrhosis and liver failure. However, patients with NAFLD universally have hepatic insulin resistance, placing them at high risk of developing glucose intolerance and Type 2 diabetes.
Because no pharmacotherapy exists to directly deplete hepatic fat infiltration, diet intervention is currently the mainstay therapy for improving fatty liver in children and adolescents. Dietary guidelines for the treatment of pediatric NAFLD are not specific, and generally recommend avoidance of calorically dense foods.
“Our pilot study in 23 adolescents with NAFLD suggests that a weight-maintaining, low-glycemic, moderately carbohydrate-restricted diet significantly improved both hepatic steatosis and hepatic insulin sensitivity,” Goss said.
The grant will help fund a randomized controlled trial to examine the effects of a weight-maintaining, moderately carbohydrate-restricted versus fat-restricted diet on changes in hepatic lipid content. The effects will be assessed with magnetic resonance imaging and spectroscopy following a 12-week controlled feeding phase and a 12-week free-living phase in adolescents with NAFLD. Groceries will be provided to families for 12 weeks.
“Results from this study will further our understanding of the impact of diet quality on reduction in liver fat in the absence of weight loss in pediatric NAFLD,” Goss said. “We will also probe mechanisms to determine whether reduction in liver fat in children can reduce risk of chronic disease such as Type 2 diabetes in the future.”
Funding for this grant is provided by the National Institute of Diabetes and Digestive and Kidney Disease.
