 By Erica Techo
By Erica Techo
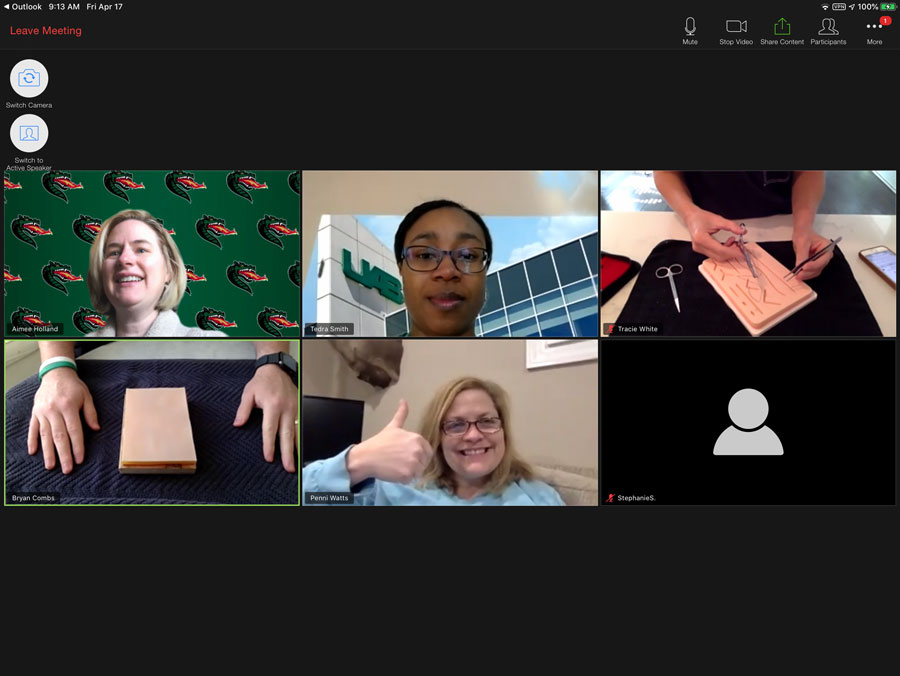
As University of Alabama at Birmingham (UAB) School of Nursing graduate students tuned into their virtual primary care skills training course in April 2020, it was not as a post-COVID-19 adjustment. Rather, their course was designed from the start as distance-accessible, thanks to funding from the UAB School of Nursing Dean’s Scholar Award.
The course will take place for a second time in June 2020, as a refresher course geared toward rural nurse practitioners.
“We actually started planning all of this in the summer of 2019, so that we could apply for the grant in August,” said Assistant Professor Tedra Smith, DNP, CRNP, CPNP-PC, CNE. “It was a bit serendipitous that we already had this planned, and we have already been able to share what we’ve learned from our first training with faculty to help them enhance what they’re doing to adapt courses during COVID-19.”
Co-investigators on the grant include Smith; Assistant Professor and Nurse Practitioner Pathways Director Bryan Combs, PhD, CRNP, FNP-BC, CNL, ATC; Assistant Professor Tracie White, DNP, CRNP, ACNP-BC, CNOR, CRNFA; Assistant Dean for Graduate Clinical Education Aimee Holland, DNP, CRNP, WHNP-BC, NP-C, FAANP; Director of Clinical Simulation Penni Watts, PhD, RN, CHSE-A and Associate Dean for Technology and Innovation Jacqueline Moss, PhD, RN, FAAN, and all worked to develop the distance-accessible course.
The motivation behind the project is to provide rural nurse practitioners with access to high-quality training and skills refreshers without some of the challenges behind an in-person course.
“For rural practitioners, it’s oftentimes difficult to travel to another location for training,” Smith said. “There are travel issues, or either finding someone to cover the office or finding a good time to close the office. If we conduct this training virtually in a short, two-hour time slot, more practitioners can take a two-hour lunch break and be able to keep their office open. This makes the training more accessible and means that rural population can continue to be seen.”
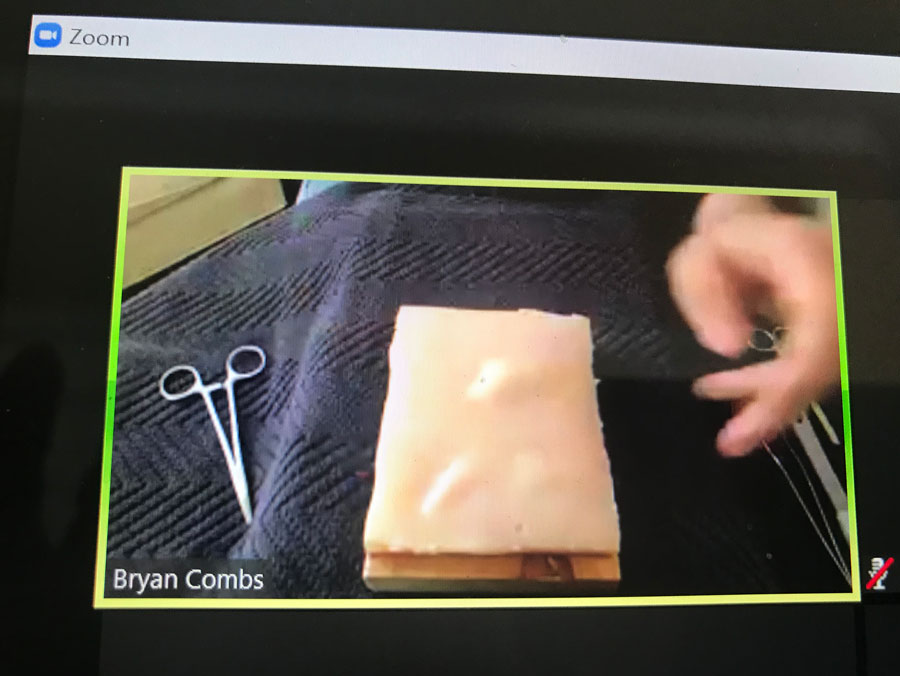 All course participants receive professionally filmed skills videos with step-by-step instructions ahead of the training course. They also receive a skills kit with needed equipment in the mail. This allows them to practice their skills and come to the course with any questions.
All course participants receive professionally filmed skills videos with step-by-step instructions ahead of the training course. They also receive a skills kit with needed equipment in the mail. This allows them to practice their skills and come to the course with any questions.
During the course, faculty focus on basic suturing and incision and draining of skin abscesses, two conditions that commonly arise in a primary care setting. Each skill is covered in about 60 minutes, with plenty of time for one-on-one interaction and a question and answer session.
Students and rural primary care practitioners will receive the same course, focused on refreshing basic skills, Smith said, in order to collect adequate responses to develop best practices for distance-accessible skills courses. Feedback from previous mini-conferences also shows this is what most attendees want.
“We did a primary care refresher mini-conference last year which received a lot of reviews,” Smith said. “99 percent of attendees were already in practice, but didn’t often have a chance to use some of the skills they learned in school. They wanted a back to basics approach, as if they were students and had never done this before, because they see these conditions and injuries less frequently than what we see in an urban setting.”
Student feedback from the April course was immensely positive, Smith said, and students thought the provided videos and instruction were helpful. Students also talked with each other as much as they would in an in-person setting, which is a positive sign for engagement.
The co-investigators chose to apply for this grant because moving skills courses online allows for greater accessibility and can save the money required to coordinate parking, meals and a physical classroom space. Having information about the best practices for virtual courses means students and nurse practitioners can benefit.
“Our students already come to campus for on-site intensives, so if we can complete some of the training online and have students on campus to validate then we can allocate time for other learning opportunities while they are on-site. I think our students will really benefit from this practice,” Smith said. “This also allows us to potentially reach more practitioners with our mini-conferences, and in the end, the patients in rural communities are going to have increased access to quality care.”
The co-investigators plan to disseminate the best practices for distance accessible skills education they develop after the June 2020 course and hope to expand the training and apply for a larger grant.
