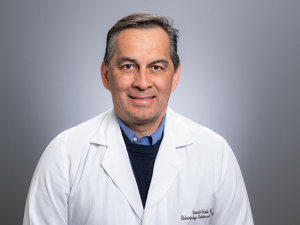
Doctors are used to speedwalking through their busy days. But it’s safe to say that Eric Wallace, M.D., medical director of Telehealth at UAB, covers more ground than most. In fact, he arrives at many of his appointments on four wheels.
 The customized, $10,000 telehealth carts that Wallace uses generally don’t move more than a few feet at a time. But they have saved Alabamians thousands of hours of driving. They are a mainstay of a UAB program that now delivers care in 64 of Alabama’s 67 counties.
The customized, $10,000 telehealth carts that Wallace uses generally don’t move more than a few feet at a time. But they have saved Alabamians thousands of hours of driving. They are a mainstay of a UAB program that now delivers care in 64 of Alabama’s 67 counties.
The UAB eMedicine team uses the carts to consult on inpatients in nine Alabama hospitals. They also treat outpatients using similar high-resolution camera systems in Alabama Department of Health offices across the state and offer rapid diagnosis of common complaints online through the UAB eMedicine Urgent Care portal.
The latest service, launched in August 2019, is at-home health monitoring for at-risk patients with diabetes, heart failure and other conditions.
These services save Alabamians time and give them better care, Wallace said. UAB eMedicine patients have saved nearly 200,000 miles and more than 3,200 hours of time spent driving to appointments, for example.
A patient who once had to drive four hours to have a wound checked post-surgery, or a dialysis checkup, can now have the same quality care at her local health department, through a secure remote link to UAB specialists.
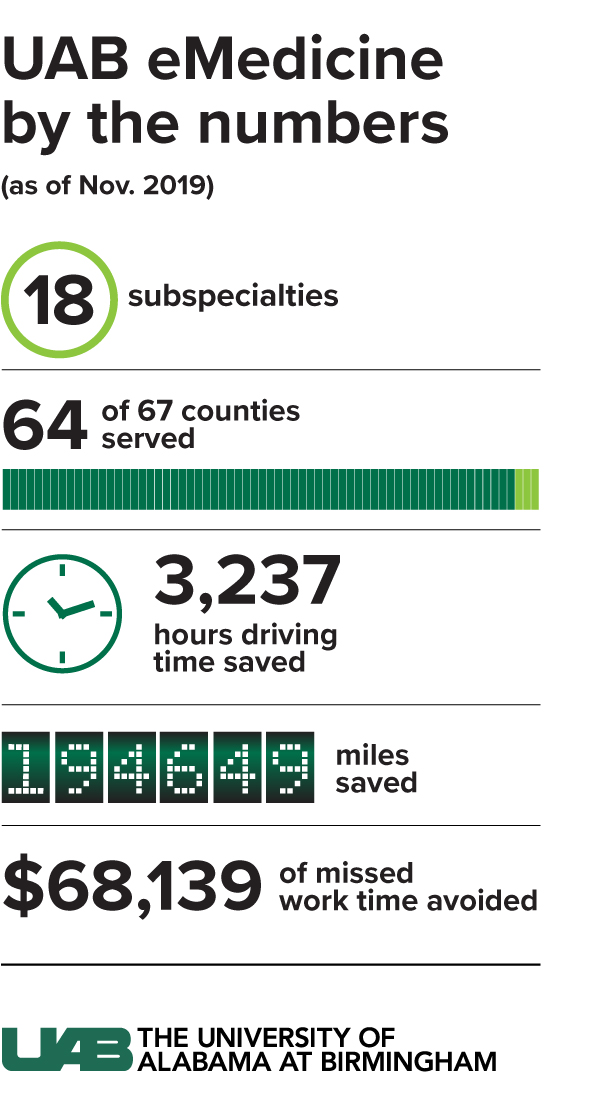 Alabama has the second-worst stroke death rate in the country, only slightly better than Mississippi. Stroke patients in rural areas once “would go to their closest ER, then wait to get transferred, putting them out of the 90-minute treatment window,” Wallace said.
Alabama has the second-worst stroke death rate in the country, only slightly better than Mississippi. Stroke patients in rural areas once “would go to their closest ER, then wait to get transferred, putting them out of the 90-minute treatment window,” Wallace said.
But telestroke care now provided by UAB at seven Alabama community hospitals means “they can get a neurologist within seven minutes.” That helps the local hospital, too, Wallace added, “because patients who were passing them by now can stay in their community for care. We’ve shown that we can keep most patients close to home.”
In late November 2019, UAB received a $750,000 grant from the U.S. Department of Agriculture to expand to more hospitals and reach more than 300,000 additional rural Alabamians. Telehealth has been generating excitement ever since it was developed in the 1960s for NASA’s Mercury space missions, Wallace pointed out. But making it work at scale, and sustainably, has been a massive challenge ever since.
“First, the tech was too expensive, which is still an issue; but it continues to get less and less expensive,” he said.
 “Then there is the issue of how you do this across medical records and work with insurers to get coverage across multiple medical records. We have solved for that. A lot of groups have done very well in one area. What we’ve managed to do in a two-year timeframe is to get the process in place to be able to offer all of this.”
“Then there is the issue of how you do this across medical records and work with insurers to get coverage across multiple medical records. We have solved for that. A lot of groups have done very well in one area. What we’ve managed to do in a two-year timeframe is to get the process in place to be able to offer all of this.”
Here's how it works:

>> 9 facilities now and expanding
>> Specialties include:
To consult with UAB, doctors at community hospitals turn to the telehealth cart, which makes specialists available at the touch of a button.
 The tools:
The tools:
Sharp vision
“I can zoom in up to 18 times,” Wallace said. “If I want to look closer at a mole, I tap that part of the screen and it zooms in automatically.”
Can you hear me now?
“Speaker volume turns out to be really important,” Wallace said. “There’s a lot of noise in an ER or an ICU. Especially when you have a patient who is a little bit hard of hearing, you need to make sure you are loud enough to get over the din.” The UAB eMedicine team has added external speakers to pump up the volume, Wallace added. “You want this to be the loudest thing in the room.”
How fast do you need?
Video requires an internet speed (technically, data transfer rate) of 3 Megabits per second (Mbps). “What we have found in general is that while internet speed can be a problem, it’s more complex than that,” Wallace said. “When eMedicine was starting, we would just analyze the internet speed coming into the hospital. However, a hospital that had 100 Mbps download speed seemed fine. But there were a thousand things using the same 100 Mbps which greatly slowed the speed used by the cart.”
The eMedicine team now has a dedicated technical team that travels to partner hospitals and works with IT staff to ensure sufficient speed is available. “And we’ve been in several discussions on the next step to link all Alabama hospitals on a high-speed network for telehealth and data transfer,” Wallace said.


>> 1,769 ambulatory visits completed as of November 2019
>> 114 visit-per-month average from June-November 2019, a 50% increase compared with the same timeframe in 2018
>> 64/67 county health departments in Alabama now have telehealth service to UAB.
When UAB physicians see a patient with a long travel time or other indication they would be a good candidate for telehealth, the patient can be scheduled for a remote appointment in their local county health department. The scheduling happens in both UAB’s and the Alabama Department of Public Health’s computer systems. After the patient arrives at the health department and has his or her vital signs recorded, “just like any doctor’s appointment,” Wallace said, nurses send the patient’s UAB physician a page. “Then the doctor makes a video call” on their computer, Wallace said, where they have secure access to the patient’s chart and test results.

Real-time health monitoring
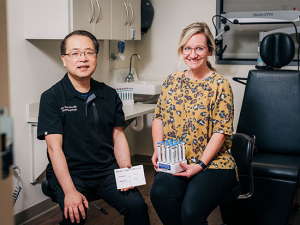
One of the newest offerings from UAB eMedicine is real-time monitoring of patients with diabetes, heart failure and COPD.
 Internet-connected scales, blood pressure cuffs, glucose meters and spirometers allow UAB eMedicine to remotely monitor at-risk patients in their homes. No internet? No problem. The equipment comes with its own internet connection.
Internet-connected scales, blood pressure cuffs, glucose meters and spirometers allow UAB eMedicine to remotely monitor at-risk patients in their homes. No internet? No problem. The equipment comes with its own internet connection.
“Say a patient is in the hospital with congestive heart failure,” Wallace said. “We can send them home with an internet-connected scale and a blood pressure cuff. Every time they step on the scale it goes to a monitor that looks at the data. If it’s above a certain level it triggers an alert and the patient gets a call to say, ‘You need to reduce your fluid intake’ or to adjust medication. Or if their blood pressure is high, the caller can ask, ‘Did you take your medicines today?’”
The pilot program, funded by grants from the UAB Health Services Foundation, is designed to give patients the resources they need to stay healthy. “This is how we keep people from needing acute care,” Wallace said.
Asynchronous care
Through its Zipnosis platform, UAB eMedicine gives patients a quick way to resolve more than 20 common medical problems.
 Patients spend about 15 minutes answering questions on an online form, then generally receive a treatment plan from a UAB provider within an hour during the business day.
Patients spend about 15 minutes answering questions on an online form, then generally receive a treatment plan from a UAB provider within an hour during the business day.
The service can be used for colds, sinus infections, flu, urinary tract infections, vaginal yeast infections, pink eye and more.
The pilot program, funded by grants from the UAB Health Services Foundation, is designed to give patients the resources they need to stay healthy. “This is how we keep people from needing acute care,” Wallace said.
Synchronous care
Coming this year, UAB eMedicine plans to launch an urgent care service that will allow patients to chat with a physician over video in real time.
“Patients and docs want to do it both ways,” Wallace said. “Sometimes you want to handle it with a quick email, other times you need the video experience. We just want the care out there, whatever is easiest for the patient.”
The future
Despite the fact that he is surrounded by the latest health tech all day — or perhaps because of it — Wallace is quick to point out that technology has its limits. “We’ve been in hospitals where there are four different carts,” he said. “Every time they added a new specialty, they got a new cart, which means everyone had to learn a new system. But people can only learn so much technology before they shut down and say, ‘I’m not going to do this anymore.’ Not to mention that it’s inefficient and can provide undue delays in care.”
Wallace’s vision is to be able to offer a single cart that can provide partner hospitals “with any specialty they need,” he said. “If you have stroke and want to add critical care, it’s just a matter of adding a button on the screen. At some point I imagine we’ll have 10 buttons, and any thing we can do here you’ll be able to do over there.”
Grants from the USDA, Alabama Department of Public Health and Appalachian Regional Commission, along with awards from the Daniel Foundation and other groups, have been instrumental in providing equipment and launching services. Wallace is particularly proud of the viable economic model that UAB eMedicine has developed, however. “A lot of programs have lived and died by their grants,” he pointed out. “That is not what we’ve stood up here. We are financially viable with or without the grants.”