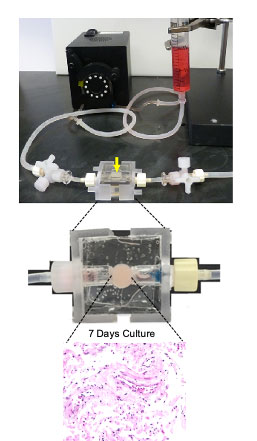
 This bioreactor from the Deshane lab can keep human lung cells alive for at least two weeks. Its detailed model of human lung tissue and its response to SARS-CoV-2 provides a test bed for studying new therapies. It is clear that SARS-CoV-2, the novel coronavirus that causes COVID-19, causes widespread havoc in human lungs. How that process works in detail, however, remains fuzzy. A particular challenge is to understand the out-of-control immune reaction to the SARS-CoV-2 infection known as cytokine storm, which has been implicated in many of the deaths from COVID-19.
This bioreactor from the Deshane lab can keep human lung cells alive for at least two weeks. Its detailed model of human lung tissue and its response to SARS-CoV-2 provides a test bed for studying new therapies. It is clear that SARS-CoV-2, the novel coronavirus that causes COVID-19, causes widespread havoc in human lungs. How that process works in detail, however, remains fuzzy. A particular challenge is to understand the out-of-control immune reaction to the SARS-CoV-2 infection known as cytokine storm, which has been implicated in many of the deaths from COVID-19.
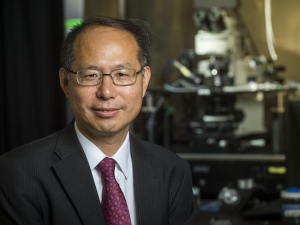
"It is vital to understand the pathogenesis of the disease and these cytokine storms — we really need a window on that," said Jessy Deshane, Ph.D., associate professor in the Division of Pulmonary, Allergy and Critical Care Medicine. "But at the moment we don't have any good models to study the disease.” Animal models take a long time to establish, she noted, “and the previous experience with the original SARS showed that these models cleared the virus quickly," unlike in humans.
Deshane is exploring an alternate approach as one of 14 recipients of pilot funding from the School of Medicine and its Precision Medicine Institute. The Deshane lab has projects on immune suppression in lung cancer and has been studying environmental exposures and asthma exacerbations for several years. "We study this in people, but it's difficult when you have to schedule a lung aspiration procedure every time," Deshane said.
Living lungs in the lab
Searching for a better method, Deshane turned to tissue-engineered, 3D human-tissue models — small pieces of human tissue, kept alive for weeks, during which time researchers can perform detailed experiments. Her postgraduate fellow, Kayla Goliwas, Ph.D., has a great deal of expertise in developing these platforms for breast-cancer cell lines and lung-cancer tissues.
| "It's a little culture platform, with a round piece of tissue, 5 millimeters in diameter, that is connected to a pump that continuously perfuses the piece of tissue with nutrients to keep the cells viable. We can sustain the tissues for at least two weeks, and there is no indication we couldn't go longer." |
"It's a little culture platform, with a round piece of tissue, 5 millimeters in diameter, that is connected to a pump that continuously perfuses the piece of tissue with nutrients to keep the cells viable," Goliwas said. "We can sustain the tissues for at least two weeks, and there is no indication we couldn't go longer." Each piece of tissue can be used to create four to eight bioreactors for testing.
But you can't simply collect a snippet of human lung tissue from a volunteer. So Deshane has established a collaboration with James Donahue, M.D., a UAB thoracic surgeon who removes tumors from patients with lung cancer. To be sure that they have removed all of a tumor, surgeons take out a small section of healthy tissue on the margins of the tumor site. "We worked out a protocol to get tissues when they do lung cancer resections," with the patient’s consent, Deshane said. "We get the uninvolved tissues that don't have tumor."
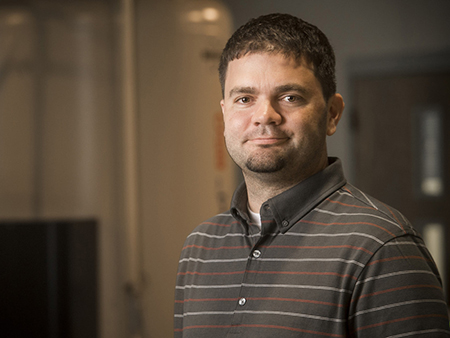
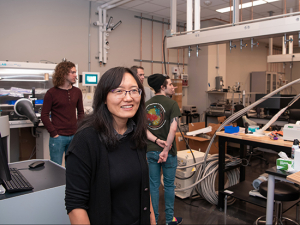
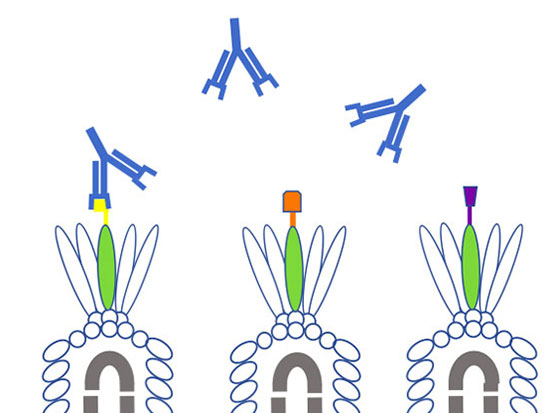
 Jessy Deshane, Ph.D. (left), associate professor in the Division of Pulmonary, Allergy and Critical Care Medicine, and her postgraduate fellow, Kayla Goliwas, Ph.D. (right), are pioneering new territory in the study of SARS-CoV-2 and its effect on lung cells.Deshane realized that these tissue models could open a path to detailed studies of how SARS-CoV-2 infects the lungs. They also could offer new insight on how the immune system responds to those infections, she said. "We've shown that in normal lung tissue we can maintain different kinds of cell populations, including epithelial cells, endothelial cells and immune cells, that are present in the lungs," Deshane said. "We are able to see T cells in the lung tissue and maintain them.” One theory of cytokine storms is that T cells become hyperactivated and eventually become exhausted, making them ineffective at stopping viral infection. “You can study this local response,” Deshane said. “What are the T cells doing? How is this virus eliciting the cytokine storm? Are there other cells getting infected in the lung?"
Jessy Deshane, Ph.D. (left), associate professor in the Division of Pulmonary, Allergy and Critical Care Medicine, and her postgraduate fellow, Kayla Goliwas, Ph.D. (right), are pioneering new territory in the study of SARS-CoV-2 and its effect on lung cells.Deshane realized that these tissue models could open a path to detailed studies of how SARS-CoV-2 infects the lungs. They also could offer new insight on how the immune system responds to those infections, she said. "We've shown that in normal lung tissue we can maintain different kinds of cell populations, including epithelial cells, endothelial cells and immune cells, that are present in the lungs," Deshane said. "We are able to see T cells in the lung tissue and maintain them.” One theory of cytokine storms is that T cells become hyperactivated and eventually become exhausted, making them ineffective at stopping viral infection. “You can study this local response,” Deshane said. “What are the T cells doing? How is this virus eliciting the cytokine storm? Are there other cells getting infected in the lung?"
Testing potential therapies
A detailed model of human lung tissue and its response to SARS-CoV-2 also provides a test bed for studying new therapies. "This lets us study treatments — which drugs are better?” Deshane said. “Can you use protease inhibitors? Camostat mesylate has worked really well in in vitro studies, for example. Can you use that in combination with other therapies?"
As part of her COVID-19 research project, Deshane plans to test some of the top potential therapies identified by researchers in the Precision Medicine Institute, who are using artificial intelligence and computer simulations to predict which FDA-approved drugs may be effective against SARS-CoV-2.
‘Whole new world’
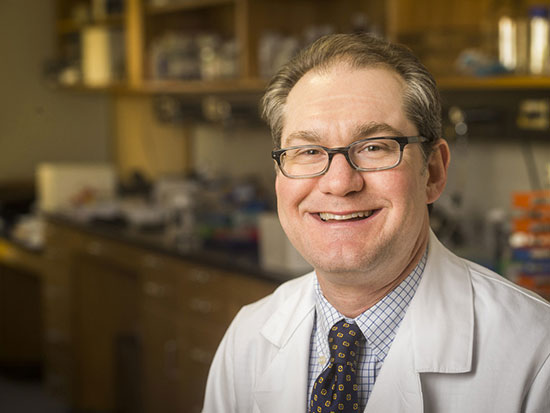
Studying ongoing viral infection with SARS-CoV-2 requires a number of protections — plus a reliable source of the virus. These are all available through Deshane’s collaboration with Kevin Harrod, Ph.D., professor in the Department of Anesthesiology and Perioperative Medicine. (See related story.) "Anything that is infected has to stay there" in Harrod’s lab, Deshane said. "We had to assemble a whole set of components for our three-dimensional tissue model that will be staying there and not coming out until the project ends."
| "It is vital to understand the pathogenesis of the disease and these cytokine storms — we really need a window on that. But at the moment we don't have any good models to study the disease.” |
In addition to building the model system, Goliwas is being certified for work in high biosafety environments. "She can take the circulating fluid out, and we can measure cytokines, et cetera, that the cells release," Deshane said. "We will be able to have a readout on the virus-related toxicity and how infection affects this entire lung-tissue system."
This line of research "is a whole new world for us," Deshane added. "In some ways it is a huge leap and is very exciting. But a lot of what happens to the lymphocytes and T cells in COVID-19 occurs in the cancer world as well. I think it's going to give us new answers to how we can help people with lung cancer."
Read more on UAB's urgent COVID-19 research projects

Glow-in-the-dark coronavirus testing is first project of new hire

Tackling his third pandemic, UAB researcher gets up close with coronaviruses in order to kill them

Researchers are creating a coronavirus showdown to settle pressing antibody problems
Where are the good antibodies against COVID-19? UAB project aims to find out
Helpful viruses may unlock the secrets of coronavirus antibodies
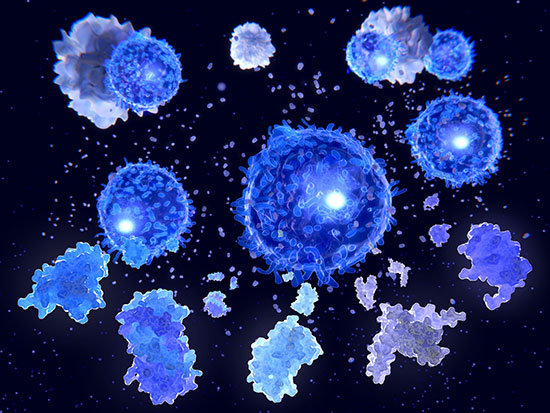
Cytokine storm treatment for coronavirus patients is focus of first-in-US study