 For most of us, weight gain is gradual – but it adds up over our adult years. A new study is testing whether daily self-weighing on a scale that graphically tracks weight over time can help prevent weight gain.
For most of us, weight gain is gradual – but it adds up over our adult years. A new study is testing whether daily self-weighing on a scale that graphically tracks weight over time can help prevent weight gain.
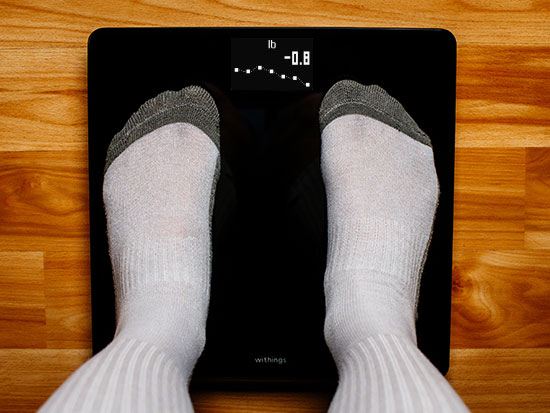
STEVE WOOD | University RelationsStep on the scale each morning and what do you get? Over the next two years, UAB researchers are answering that question in a study testing the power of low-effort interventions to manage weight.
Obesity researchers usually create and study comprehensive, intensive interventions that involve significant interaction between patients and intervention staff. “That’s the gold standard approach to getting clinically meaningful amounts of weight off,” said Gareth Dutton, Ph.D., professor in the Division of Preventive Medicine in the UAB Heersink School of Medicine. But in the real world, those “staff and resources aren’t available,” Dutton said. “We wanted to identify lower-intensity, more targeted approaches that could help people manage their weight effectively and not be so burdensome.”
Simply maintaining weight would be a success because America’s obesity problem is getting worse all the time. Each year, American adults gain 1 to 2 pounds on average. “For most of us, that weight gain is very gradual; but it accumulates and increases the risk of chronic conditions” — everything from diabetes to high blood pressure and cancer, said Kevin Fontaine, Ph.D., professor and chair of the Department of Health Behavior in the School of Public Health.
“The idea is that, if people regularly engage and get that visual feedback to see how their weight is changing over time, will that prevent weight gain?”
Daily self-weighing
In a new study, Dutton, Fontaine and their co-investigators have removed everything but “one of the key ingredients of healthy weight management: daily self-weighing,” Dutton said. They are recruiting 400 participants, ages 19 to 75, with BMIs from 30 to 50. (Use this CDC tool to calculate your BMI using height and weight.) Half of the participants will be randomly selected to receive a Wi-Fi-enabled digital scale with a screen that graphs their weight over time. The scale also connects to a smartphone app. The other participants will receive a gift card worth the same amount as the scale ($60) to purchase weight-maintenance supplies.
To learn more about the SWOP study, email swop@uabmc.edu.
“The truth is we’re not really good at getting people to lose weight,” said Fontaine, who is the Antoine Lavoisier Endowed Professor of Energetics and Healthy Lifestyles at UAB. “It seems kind of like giving up to switch the goal to not gaining weight, but this is something that could be rolled out widely and have reverberating effects.”
“We wanted to identify lower-intensity, more targeted approaches that could help people manage their weight effectively and not be so burdensome.”
Study tracking outcomes, costs
“The idea is that, if people regularly engage and get that visual feedback to see how their weight is changing over time, will that prevent weight gain?” Dutton said. And is the difference meaningful enough to outweigh the cost of the scale itself? Their two-year study, known as Daily Self-Weighing for Obesity Management in Primary Care, or SWOP, aims to gather that data. The researchers will track changes in body weight across the two groups at six, 12, 18 and 24 months, along with their health care utilization at those same time points, among other measures.
“I’ve got a lot of students who are studying for the MCAT [medical school entrance exam],” Fontaine said. “They take all these practice tests to get immediate feedback on how they are doing, and they can make these microadjustments to hit their target. We think the same thing may happen with daily self-weighing.”
“The initial in-person visit is very short, and the follow-up visits are relatively low-commitment, just as the treatment is low-commitment. People are hesitant about anything that involves time and effort, but this is short and safe.”
Automated as much as possible
In addition to the age and BMI requirements mentioned above, study enrollees must be receiving care at one of the study’s participating primary care clinics and have a smartphone and Wi-Fi at home. They do not need to figure out how to set up the scale on their own, however. The research team works with participants by Zoom and phone to get everything set up. “We hand them the scale and get on a Zoom call to walk them through the process,” Dutton said. “Once it is set up, they don’t have to think about it for the next two years except for stepping on the scale each morning. There is nothing to track on a piece of paper. It tracks the weight and emails the feedback and graphs. We tried to automate the process as much as possible.”
“Because of the design of this project, it adapted relatively easily to COVID and remote measurements,” said Amy Dobelstein, program manager in the Division of Preventive Medicine. “The initial in-person visit is very short, and the follow-up visits are relatively low-commitment, just as the treatment is low-commitment. People are hesitant about anything that involves time and effort, but this is short and safe.”
To learn more about the SWOP study, email swop@uabmc.edu.
