You’ve heard it from kindergarten teachers, self-help books, and significant others: You’re one of a kind. Unique from head to toe.
Now you’ll hear that from your physician. Because the era of precision medicine is here.
What is precision medicine? Consider your next-door neighbor. You may share a fence, a ZIP code, and a love of cookouts. Perhaps even a diagnosis of high blood pressure. But your treatments might not be the same, all because of one gene mutation that makes Treatment A more effective for you, while Treatment B works better for her. The goal of precision medicine is to discover your unique attributes and mold health care to match your needs. It’s a revolutionary approach: The patient becomes the source of solutions for predicting, preventing, and treating disease.
UAB has leaped into a leading role in precision medicine, making the dream of truly individualized care a reality for Alabamians today. Follow along as we share some early successes and look ahead to exciting breakthroughs that could help you live your one-of-a-kind life to the fullest.
Finding the origin of the solution
“Matt Might” sounds like a superhero’s name. He certainly is one to his son Bertrand, born with a mysterious disease that not only caused pain and seizures, but wouldn’t even allow him to cry. He could wail, but no tears would come.

The "first wave" of precision medicine
has focused largely on diagnosing disease. UAB's vision is to set the standard for using precision medicine to treat disease, says Matt Might.
After years of traveling to clinics to seek a diagnosis, Matt Might, his wife Cristina, and Bertrand all underwent exome sequencing—DNA sequencing that focuses on the expressed genes in a genome. There they found their answer: Bertrand had mutations that had destroyed the function of the NGLY1 gene. Bertrand “was the first human ever diagnosed with missing this gene and having it linked to a disease,” Might says. “Then the question became, can we treat it?”
Might, a Ph.D. and computer science expert, applied his knowledge of viral marketing, search engine optimization, and social media to seek others like Bertrand. Online, Might found families struggling with NGLY1 deficiency and scientists volunteering to search for potential therapies. Together, they learned that without a functioning NGLY1 gene, Bertrand and the others are deficient in a glucose derivative called N-acetylglucosamine—which can be purchased on Amazon. After testing it on himself, Might began giving it to Bertrand. Three days later, Bertrand was crying—with actual tears rolling down his face. The mighty Mights had won their first battle. And Matt Might was ready to harness the power of precision medicine to help other families searching for answers.
Last year, Might became the inaugural director of UAB’s Hugh Kaul Precision Medicine Institute, bringing stellar credentials to Birmingham. President Barack Obama appointed him to the White House Precision Medicine Initiative in 2015. He also held faculty positions at the University of Utah, where he specialized in computer science and pharmaceutical chemistry, and Harvard Medical School, where he was a visiting professor of biomedical informatics. His goal is to use computational technologies such as genomic sequencing to discover the best way to treat a specific person’s disease. “I tell people I’m developing the algorithm for precision medicine,” he says. “The input is the patient.”
The road ahead
The “first wave” of precision medicine has focused largely on diagnosing disease. UAB’s vision is to set the standard for using precision medicine to treat disease, says Matt Might.Might outlines the future growth of precision medicine:
1. From rare to everywhere: “Rare disease and cancer will benefit the most in the near term. We need the genomic arsenal being assembled in rare disease to construct drug cocktails needed for precision medicine in diseases like diabetes, depression, and heart disease. Eventually, all fields will benefit from this data-driven approach.”
2. Not just genetics: “The bulk of precision medicine now is genomic medicine. But going forward, all personal health data will be used to optimize a patient’s care—potentially even data from cellphone health apps and fitness trackers. The resulting treatment could be a targeted medication or a targeted lifestyle change.”
3. Access for everyone: “Bringing the full benefit of precision medicine to all—especially underserved communities—requires precision delivery. In some cases, this means we bring the care to the community. For example, for a precision cancer prevention program, we may need to work with local stakeholders who bring mobile clinics to community institutions and events.”
Might says he is “terrifically excited” to be at UAB, with its “constellation of resources” and partnerships that place Alabama ahead of the curve in bringing precision medicine to patients. Supported by the Hugh Kaul Foundation’s $7-million investment in the institute, Might is recruiting research leaders “to get the right drug to the right patient at the right time.”
Precision medicine will reshape the search for those drugs, as in Bertrand’s case. “A big component is repurposing—testing the library of several thousand Food and Drug Administration-approved drugs to find out if they have other effects that are clinically beneficial, for diseases they were never originally intended to treat but actually do,” Might explains. He also foresees a more customized approach to the discovery and development of new drugs—one driven by patients armed with genetic data.
“We’ve established a blueprint for using precision medicine to go from disease discovery to therapeutic identification within one year,” Might says. “At UAB, we’re scaling it up in a big way.” This means that someday soon, he adds, no patient or family will hear a clinician say, “There is nothing we can do.”
Sequence of breakthroughs
Cancer is a disease with a thousand faces. Take breast cancer, for example. It’s not just breast cancer anymore. Instead, it might be breast cancer driven by a BRCA2 gene mutation, or breast cancer with elevated levels of the protein HER2/neu. And on and on.
The goal of precision oncology, says Eddy Yang, M.D., Ph.D., is to pinpoint these specific defects—to recognize the face within each patient. Yang is the ROAR Southeast Cancer Foundation Endowed Chair in Radiation Oncology, vice chairman for translational science in the Department of Radiation Oncology, associate program leader of experimental therapeutics in the Comprehensive Cancer Center, and deputy director and associate director for precision oncology in the Hugh Kaul Precision Medicine Institute.
Precision oncology is nothing new at UAB’s trailblazing Comprehensive Cancer Center. Beginning in 2013, Yang has met each month with fellow clinicians and scientists to review records of patients whose advanced cancer isn’t responding to traditional therapies. Then the group, the Molecular Tumor Board (MTB), decides whether to send cases out for genetic sequencing to help identify a new course of action.
One patient, Yang recalls, had salivary gland cancer, and had run out of treatment options. But DNA sequencing ordered by the MTB identified an intriguing clue: The patient’s tumor had a mutation commonly seen in melanoma, a form of skin cancer. That suggested a new melanoma-based treatment option, which brought the patient remission for more than a year.
The MTB serves as a national model for incorporating precision oncology into standard practice—and has yielded some remarkable results. Still, “sequencing isn’t a magical cure,” Yang notes. “We’re not going to find drugs for every person whose tumor we sequence, but we may be able to offer better treatment options for some patients.” Drug development is happening at such a rapid pace that a few extra months can make a big difference. “Sometimes we’re trying to buy patients enough time to get to the next new treatment,” Yang says.
Through a partnership with Michigan-based Strata Oncology, UAB cancer patients with tumors that can’t be removed surgically or that have spread to another part of the body can receive no-cost tumor sequencing. The trial is also available to all glioblastoma and pancreatic cancer patients, although any tumor type is eligible.
“We now sequence 50 to 60 patients per month” through the Strata Trial, and around 70 percent have a “tumor-driver” mutation, Yang says. Of those, around 20 percent will receive an off-label drug or be enrolled in a clinical trial of a new drug. For a sizable number, sequencing lets doctors “know what drugs not to give,” he adds. UAB patients also have access to more than a dozen new targeted therapies through another study, the TAPUR trial run by the American Society of Clinical Oncology.
UAB researchers say it’s only a matter of time before all cancers are treated based on their genomic abnormalities. “That’s the beauty of trials like Strata,” Yang explains. “For lung and colon cancer, ordering sequencing is almost reflexive for doctors. Now we can be reflexive for other types of cancer as well. Precision medicine is our standard of care.”
How cancer advances precision medicine
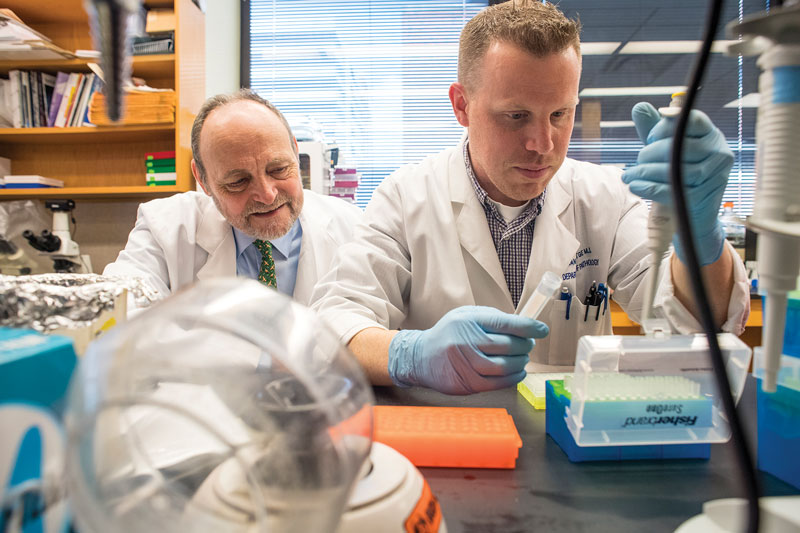
For decades, Michael Birrer, M.D., Ph.D. (at left in photo), has unraveled the molecular beginnings of gynecologic cancers. At the National Cancer Institute, and at Massachusetts General Hospital, Birrer’s lab has worked on prevention, early detection, and treatments for ovarian, cervical, and endometrial cancers based on their genomic characteristics. Now, as the UAB Comprehensive Cancer Center’s new director and the Evalina B. Spencer Chair in Oncology, Birrer is poised to play a key role in spreading the benefits of precision oncology to patients across the South.
How has this approach changed cancer treatment already?
Birrer: “Precision oncology is the poster child for precision medicine. For essentially every tumor in which scientists have validated a bonafide target and clinicians have used a small-molecule inhibitor, patient treatment has seen a huge impact. This is an exciting time in oncology—the most exciting time in my career. Things are moving very fast.
“Because these treatments are so narrowly targeted, their toxicities are narrow, which is good for patients. You may be able to change what ostensibly is a fatal disease into a chronic disease.”
How can UAB and Birmingham become precision oncology leaders?
Birrer: “We need clinical trials exploiting our molecular discoveries for every tumor type at every stage of the disease. We have about 500 patients per year on trial today; I want to increase that to 1,500 so that we become the clinical trials center for the South. That requires investment in everything from staff to space, but it benefits patients, and it could also attract major pharmaceutical and biotech companies to Birmingham.”
Alabama leads the way
The body’s genetic blueprint, containing some 6 billion characters, is remarkably similar from person to person. But major sequencing studies have shown the potential for millions of differences between individuals, sometimes as simple as the genomic equivalent of a comma where a period should be.
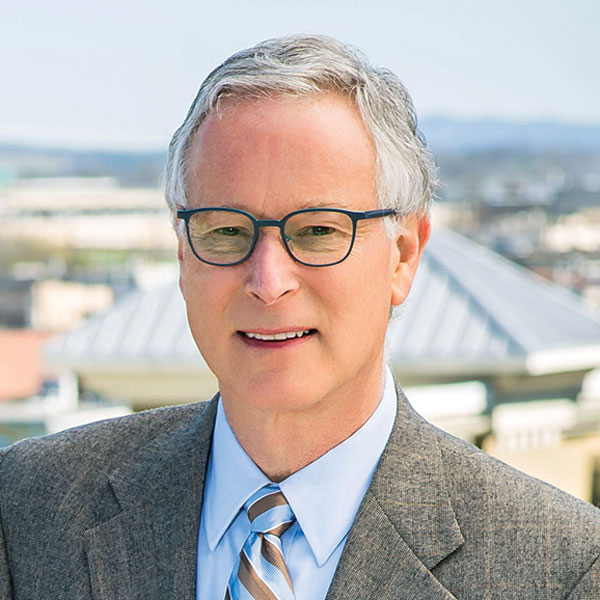 Photo by Nik Layman
Photo by Nik Layman
AGHI "will result in immediate health benefits to some participants," says Bruce Korf. The statewide quest to expand genomic medicine is among the first projects of its kind nationwide.
Most changes seem relatively benign. But which ones should raise red flags for physicians? Would entire groups of people benefit from genetic testing? When are those tests most useful?
The Alabama Genomic Health Initiative (AGHI)—among the first projects of its kind nationwide—aims to find answers as it brings cutting-edge genomic medicine to every corner of the state. It is a collaboration between the School of Medicine and Huntsville-based HudsonAlpha Institute for Biotechnology, initially funded by $2 million from the Alabama Legislature to UAB. AGHI is recruiting a diverse group of participants from every county—2,000 in the first year, with a goal of 10,000 over five years. A simple blood draw from each participant will be tested for mutations in genes where a finding can lead to potentially life-saving intervention. The collected samples also will be stored in a biobank, helping researchers to uncover new links between gene variants and disease.
This landmark project "will result in immediate health benefits to some participants,” says Bruce Korf, M.D., Ph.D., UAB chief genomics officer and the Wayne H. and Sara Crews Finley Chair in Medical Genetics. “Long term, it will help address chronic disease and rising health care costs in the state, and position Alabama at the forefront of 21st-century medicine.”
The goal is “to develop a representative cross sample of residents, broadly characteristic of ethnic, racial, and socioeconomic groups throughout the state,” adds Matt Might, who is AGHI co-director along with HudsonAlpha’s Greg Barsh, M.D., Ph.D. The data will help diversify the standard reference genome used by researchers, which is largely composed of genomes from European backgrounds, Might explains. “That is essential to bring the benefits of genetic testing to all Alabamians.”
“Technology always advances. We continually have to anticipate new ethical issues.”—Mariko Nakano, Ph.D., ethicist and assistant professor in the School of Medicine, works with bioethicists from Tuskegee University and HudsonAlpha Institute for Biotechnology to set a new standard for informed consent through AGHI.
She describes the safeguards in place for the landmark project.
Each participant’s blood sample will undergo a genotyping array test, which assesses 650,000 identified genomic biomarkers for variants in “actionable genes” identified by the American College of Medical Genetics and Genomics as linked to an established intervention. (Currently the list includes 59 genes.) “The best-known genes on the list are BRCA1 and BRCA2, associated with a risk of breast and ovarian cancers,” Korf says. Others include genes associated with risk for heart disease, hypercholesterolemia, and a life-threatening adverse reaction to certain anesthetics, among other conditions.
“I enjoy helping people understand what is truly going on with themselves or their child. I have the opportunity to empower families through education.”
—Dana Schippman, 2016 graduate of UAB’s master’s program in genetic counseling, now working at Children’s Hospital of Wisconsin.
When the results of a genetic test arrive, genetic counselors step in to provide clear explanations and answer questions. “They are on the front lines of precision medicine,” says Patricia Page, assistant professor and director for UAB’s master’s program in genetic counseling, in the School of Health Professions.
As a result, genetic counseling is a career field on the rise. The U.S. Bureau of Labor Statistics projects a growth rate of 29 percent through 2024, far outpacing the 7 percent rate for all occupations. The numbers are even better for UAB’s genetic counseling program. Graduates have a 100 percent placement rate, with many landing jobs before they matriculate. Most work in cancer genetics, followed by pediatric or prenatal genetics; others join genetic testing companies and research teams.
“We attract students from across the United States,” says Page. “We challenge them to address not only their patients’ information needs, but also their emotional and social needs.”
Participants testing positive for a variant in an actionable gene receive genetic counseling, and they can share results with their primary medical provider to discuss prevention or treatment strategies. Based on previous studies, the number of participants likely to get positive reports will be small—maybe 1 to 3 percent, Korf says. But “the results will be life-changing and possibly lifesaving,” he notes. “It allows family members to take appropriate action as well.”
For any person showing signs of a genetic issue of undetermined origin, experts will analyze all 22,000 genes and 6 billion DNA base pairs, a process called whole genome sequencing, at HudsonAlpha to try to uncover a gene variant offering a clue to the disease. Those participants will receive results and links to appropriate care, which could include UAB’s Undiagnosed Diseases Program (UDP). Led by Korf, the UDP has assisted more than 160 patients since its 2013 launch. More than half who have completed evaluation have received a diagnosis, the result of cutting-edge genetic technology combined with traditional strategies such as a comprehensive review of medical history and extensive interviews with patients and families. “It’s great when you can tell somebody after all this time, ‘This is what you have,’” Korf says.
In addition to AGHI, UAB is part of All of Us, a research program led by the National Institutes of Health (NIH) to gather genetic data from more than 1 million people in the United States. “It provides a chance for individuals in our region to participate in an exciting initiative intended to provide new insights into prevention, diagnosis, and management of diseases across the nation.,” Korf says.
Precision in Action
Matching medications to patients with depression, stroke, and lung disease
Click to expand
-
Finding the right treatment faster:
Although most people with depression eventually respond to some kind of antidepressant treatment, any given antidepressant has only about a one in three chance of working, says Richard Shelton, M.D., the Charles Byron Ireland Chair of Psychiatric Research in the Department of Psychiatry and Behavioral Neurobiology. “Often people give up on medication after trying treatments that don’t work. In worst-case scenarios, the person may commit suicide.” Shelton was part of a research team discovering mutations on genes linked to depression and drug metabolism that could help doctors match patients with effective antidepressants. Now Shelton and colleagues are studying two different genetic tests that can pinpoint those mutations. They employ the tests after one or two standard medications fail to improve a patient’s depression; the results offer guidance on which drug to try next. The group also participates in large-scale studies of the tests, which could make genetic considerations more common as physicians gather data to guide treatment.
Which dose is right for you?:
Strokes are all too common for African-American men and women. So too is a genetic variant, known as rs12777823, that makes a patient’s safe dose of the blood-thinner warfarin—the usual post-stroke treatment—20 percent lower than the typical dose. That discovery, from a 2013 study co-led by UAB neurology professor Nita Limdi, Pharm.D., Ph.D., is a key finding in the burgeoning field of pharmacogenetics, which aims to find links between patients’ genes and their response to drugs. “Forty percent of African-American patients we see in clinic at UAB have that [warfarin] marker,” Limdi says. Eventually, she believes, genetic tests will be commonplace before doctors write a prescription. For now, widespread implementation—and insurance reimbursement—depends on more research at major hospitals like UAB. “Years from now we might have this information on everybody,” says Limdi. “For now, let’s figure out who is most likely to benefit and build interventions.”
Circles of life:
Lab-grown “mini lungs” could provide a fresh approach to finding effective drugs for patients with a devastating lung disease. Pulmospheres—one-millimeter-wide spheres containing all cell types found in a human lung—“simulate the lung’s microenvironment,” says Veena Antony, M.D., professor in the Division of Pulmonary, Allergy, and Critical Care Medicine. In a first-of-its-kind, National Institutes of Health-funded study, Antony and colleagues grew pulmospheres from patient biopsy lung tissue. Then they observed how the spheres reacted to two FDA-approved medications that slow the progress of idiopathic pulmonary fibrosis (IPF), a life-threatening disease that causes lung tissue to stiffen and scar. Within 16 hours, they could see whether the spheres responded. “A reliable clinical test to predict which drug works best for which patient is urgently needed,” Antony says. Pulmospheres also could help gauge the effectiveness of potential IPF drugs in development.
Intelligent medicine

As precision medicine reshapes treatment, it also will change UAB’s skyline. The Genomic Medicine and Data Sciences Research Building, scheduled for a 2018 groundbreaking, will house scientists and advanced technology and create hundreds of new jobs. The facility will complement the Hugh Kaul Human Genetics Building, home to an interdisciplinary team focused on research, patient care, and genetic testing. The groundbreaking comes 56 years after the School of Medicine opened the Southeast’s first medical genetics program, founded by Sara Will Crews Finley, M.D., and Wayne H. Finley, M.D., Ph.D.
Precision medicine is powered by information—minute details about patient genomes, medical and family history, lifestyle, environment, and so forth. Then there are the reams of medical research published each year—in 2014, there were 3 million new studies published on cancer alone. In that deep ocean of data, how will your doctors find the droplet of knowledge that helps them determine the most effective treatment for you?
They’ll identify it through informatics, or “the art and science of organizing knowledge of human health and disease, and making it useful for problem solving,” explains James Cimino, M.D., director of UAB’s Informatics Institute and the School of Medicine’s Endowed Professor in Informatics. In practice, that involves having a librarian’s fixation on order and classification, and a physician’s eye for picking out key details and observations.
Cimino has both. As a pioneering digital physician, he helped build DXplain, a landmark diagnostic support program used in medical schools, and invented infobuttons, smart links embedded in a medical record that offer vital context—contraindications or dosing guidelines when a doctor orders a new drug, for example. Cimino came to UAB in 2015 from the NIH, where his Laboratory for Informatics Development designed a system to let researchers query four decades of research data to find new insights and developed a method to link patients’ genomic data to their electronic health records.
Cimino has assembled a formidable team of UAB researchers to take on a similar challenge. “You can’t just collect data and expect it to speak for itself,” says Jake Chen, Ph.D., who joined the Informatics Institute in 2016 as associate director and chief bioinformatics officer. “It is challenging to sift through unless you have informatics practices—computers, prior knowledge databases, experts who know what they are looking for.” Ultimately, informatics will give researchers and clinicians more power to model complex diseases and observe outcomes of experimental therapies prior to human clinical trials, he says.
“Genetics is the science of this century, and it will eventually permeate all areas of medicine.”
—Jordan Barham, genetics and genomic sciences major
Rapidly evolving technologies are creating strong demand for new types of academic training. Last fall, UAB’s College of Arts and Sciences debuted two new undergraduate majors—immunology, and genetics and genomic sciences—which are among only a handful available at American universities. Both programs combine lectures from world-renowned UAB researchers with opportunities to work alongside them in their labs.
Barham, a junior on the women’s soccer team from Woodstock, Georgia, works in the lab of Marek Napierala, Ph.D., in the Department of Biochemistry and Molecular Genetics, studying the rare genetic diseases Friedrich’s ataxia and Wolfram syndrome. Cameron Lafayette, a senior from Columbus, Georgia, plans to pursue an M.D./Ph.D. with a goal of becoming a pediatric neurosurgeon and cancer researcher. He works with Mick Edmonds, Ph.D., in the Department of Genetics, studying the effects of microRNAs in breast and lung cancer. Both students signed up for the new genetics and genomic sciences major as soon as it became available. “It has already had a tremendous impact on my understanding of genomic science and facilitated my lab training, furthering my passion for research,” Lafayette says.
One top project for the Informatics Institute is AGHI. Analyzing genetic information from 10,000 Alabamians generates “a lot of data to manage,” Cimino says. The information is stored in a special repository so researchers with appropriate access can use it to identify participants for future studies. “For example, they can search for people with a certain condition who fail to respond to the usual therapy, and then obtain their genetic data to look for clues about the reason for failure,” says Cimino, who also co-directs UAB’s Center for Clinical and Translational Science. “Since many subjects will be UAB patients, researchers can access clinical data as part of their electronic health records.”
The transformative power of informatics lies in “intelligent medicine”—connecting the deep knowledge of biological systems from basic science researchers with the clinicians who can put it into practice, Chen says. “Informatics is really a discovery hub.”
Editorial contributors: Ryan Broussard, Kendra Carter, Cary Estes, Jane Longshore, Bob Shepard, Sarah C.P. Williams
Published March 2018

 Photo by Nik Layman
Photo by Nik Layman