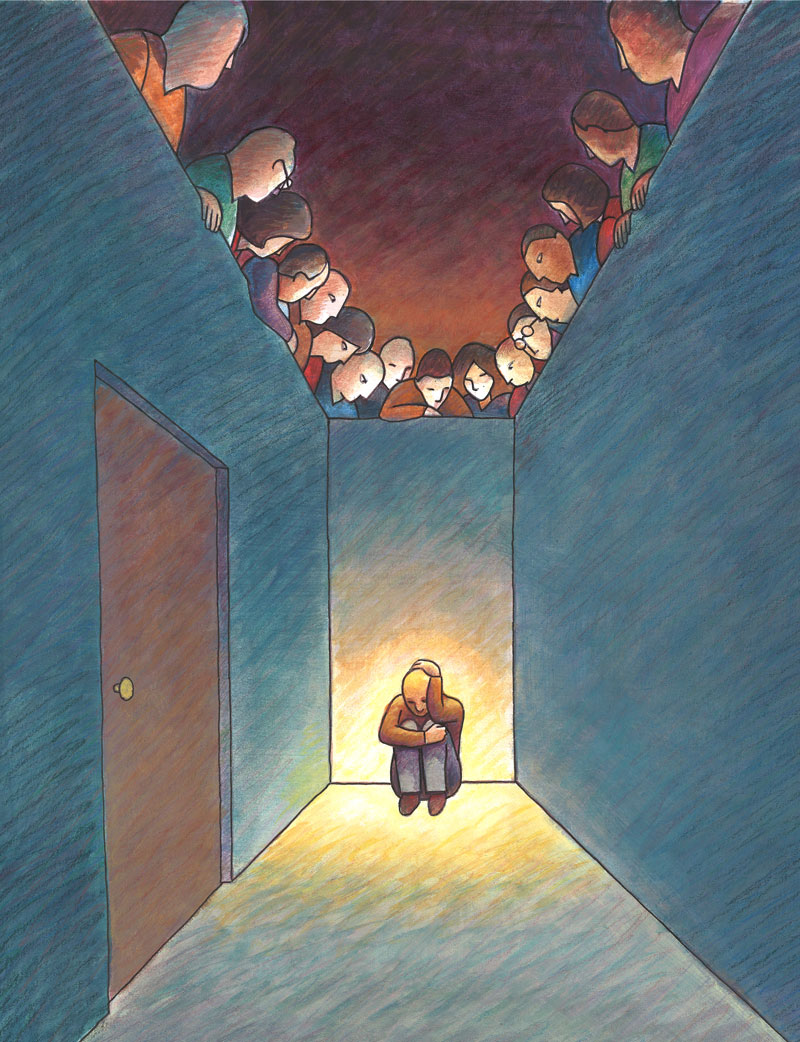
In a rural Alabama town, an HIV-positive woman struggles to get treatment without being seen. If she visits the nearest clinic, the odds are good that she’ll run into someone she knows. The clinic is located on a main street across from a popular auto-repair shop, where men line the street, watching. So she concocts a story about needing to shop at a mall in Montgomery, more than an hour away. An acquaintance offers her a ride to the mall, where she arranges for staff from a Montgomery HIV clinic to pick her up and bring her back after her scheduled appointment.
This woman is not fictional, and her secretive efforts aren’t unusual. “There are countless stories like this,” says Mirjam-Colette Kempf, Ph.D., M.P.H., a professor in the UAB School of Nursing. “You can imagine the barrier to care in small, close-knit communities when there’s this stigma making you want to hide your disease.”
Stigma against HIV, depression, herpes, psoriasis, chlamydia, unwanted pregnancies, and many other conditions and diseases—even some types of cancer—can limit health care and positive outcomes for patients. The fear of being shamed and shunned pushes people to travel hours to clinics, but it also may lead them to avoid treatment altogether by refusing diagnostic tests, physician visits, or prescribed medicines. Some individuals isolate themselves. Others choose to ignore their illness, putting entire communities at risk for the spread of disease.
UAB researchers, including Kempf, are chipping away at stigma’s invisible barrier. They’re trying to understand what drives it, what health-care providers can do to help patients step out of the shadows, and what solutions could break the links tying shame and fear to poor health.

Different People, Diverging Reactions
Bulent Turan, Ph.D., assistant professor of psychology in the UAB College of Arts and Sciences, describes stigma as “a social process, in which people who don’t have a condition perceive those with a condition as being inferior, as having a character flaw.” It crosses genders, income classes, races, sexual orientations, and borders. But it takes different forms, adds Turan, who mostly studies stigma as it relates to HIV. It can show up as an overt act of discrimination—an HIV-positive patient left by a spouse or denied a job. Or it can be more silent—the perceived threat of discrimination and judgment that a patient senses and internalizes.
 (Left to right) Mirjam-Colette Kempf, Bulent Turan, and Janet Turan have developed interventions designed to break down barriers of HIV stigma from Alabama to Africa.
(Left to right) Mirjam-Colette Kempf, Bulent Turan, and Janet Turan have developed interventions designed to break down barriers of HIV stigma from Alabama to Africa.“All these dimensions of stigma can play out in different ways,” Turan says. “And individuals respond differently to feeling stigmatized.”
For example, in another Alabama town, miles away from the woman who relies on cover stories to obtain HIV treatment, Kempf met a woman who had the opposite reaction to her diagnosis. “The day she heard she was HIV-positive, she told her boss and then called her entire five-generation family and sat them down and told them,” Kempf recalls. “Stories like that are what we’d like to see, but right now, they’re the exception.”
Few predictors can reveal whether a patient will fly in the face of stigma or retreat. Even in areas of Africa where HIV rates are high—where most people likely know someone with the disease—the shame felt by patients remains, says Janet Turan, Ph.D., professor of health care organization and policy in the UAB School of Public Health (and Bulent Turan’s wife and research partner), who has spent a decade working with HIV-positive women in sub-Saharan Africa.
“Even when HIV is common, the moral judgment and blame that go along with it don’t go away,” says Janet Turan, who was invited to speak at the White House about HIV stigma in 2016. Understanding what separates those communities and patients from others better able to deal with stigma can help researchers design interventions, she adds.

The Dangers of Shame
To quantify how much stigma HIV patients experience, and what contexts it appears in, Bulent Turan spearheaded a study that used smartphones to track patients’ experiences three times a day for a week. Patients who reported more stigma and discrimination, he found, also ranked higher on scales of depression. Moreover, these same patients were the least likely to adhere to their medication regimens and appointments.
It’s a finding that both Turans have discovered repeatedly—in areas from Africa to Alabama. And it isn’t only true for HIV. Jackie Feldman, M.D., professor emerita of psychiatry in the UAB School of Medicine, says many patients with depression, anxiety, schizophrenia, or other psychiatric disorders are plagued by stigma.
“They’re reluctant to identify themselves as living with a mental disorder,” she says. “It may make them not be honest about symptoms, withdraw from family and friends whom they’re worried might judge them, and suffer from decreased social and work opportunities.”
The same ideas are echoed by Edward Hook III, M.D., professor of infectious diseases in the School of Medicine, who studies the stigma associated with sexually transmitted infections. “We spend more money on health care than any other nation on earth but have higher rates of some sexually transmitted diseases (STDs),” says Hook. “Stigma plays a central role in that. It keeps people from getting tested and seeking treatment.” When patients don’t get tested, he says, they continue to infect others without knowing it.
In 22 countries, more than 10 percent of people living with HIV reported denial of health care. More than 1 in 10 people living with HIV reported that they had been refused employment or a work opportunity because of their HIV status in the preceding 12 months.
Source: People Living with HIV Stigma Index, Global AIDS Update 2016, UNAIDS
Source: People Living with HIV Stigma Index, Global AIDS Update 2016, UNAIDS
More than 50 percent of people ages 15-49, surveyed in multiple countries between 2009 and 2014, reported they would not buy vegetables from a shopkeeper living with HIV.
Source: Global AIDS Update 2016, UNAIDS: Joint United Nations Programme on HIV/AIDS
Source: Global AIDS Update 2016, UNAIDS: Joint United Nations Programme on HIV/AIDS
Only 25 percent of U.S. adults ages 18-24 believed that a person with mental illness can eventually recover.
Source: HealthStyles survey, 2006, Substance Abuse and Mental Health Services Administration and Centers for Disease Control and Prevention
Source: HealthStyles survey, 2006, Substance Abuse and Mental Health Services Administration and Centers for Disease Control and Prevention
-
In 22 countries, more than 10 percent of people living with HIV reported denial of health care. More than 1 in 10 people living with HIV reported that they had been refused employment or a work opportunity because of their HIV status in the preceding 12 months.
Source: People Living with HIV Stigma Index, Global AIDS Update 2016, UNAIDS -
More than 50 percent of people ages 15-49, surveyed in multiple countries between 2009 and 2014, reported they would not buy vegetables from a shopkeeper living with HIV.
Source: Global AIDS Update 2016, UNAIDS: Joint United Nations Programme on HIV/AIDS -
Only 25 percent of U.S. adults ages 18-24 believed that a person with mental illness can eventually recover.
Source: HealthStyles survey, 2006, Substance Abuse and Mental Health Services Administration and Centers for Disease Control and Prevention -
An estimated 20 million new sexually transmitted infections occur annually in the United States, but only about 2 million total cases of chlamydia, gonorrhea, and syphilis were reported in 2015.
Source: Sexually Transmitted Disease Surveillance, 2015, Centers for Disease Control and Prevention
Wounding Words
When you think about someone stigmatizing a disease—be it an STD or cancer—you likely imagine the person being judgmental and discriminatory as an uneducated uncle, the kind of guy making loud, colorful remarks at the Thanksgiving table. But stigma can be just as prevalent among doctors, nurses, and other health-care workers.
“We always assume the general public is at fault,” says Kempf. “But we as a scientific and medical community need to shoulder some of the blame.”
 Edward Hook encourages physicians and patients to talk about sexual health to help curb STD rates.
Edward Hook encourages physicians and patients to talk about sexual health to help curb STD rates.Janet Turan says she first noticed the effect of stigma in the maternity wards of sub-Saharan Africa while she was working with HIV-positive pregnant women. “We saw health-care workers themselves doing a lot of things that were stigmatizing and discriminatory,” she remembers. “Sometimes the health workers didn’t even realize the effects of what they were doing.”
Behavior she saw in Africa—which also has been observed among American health-care workers—included unnecessarily wearing gloves and face masks when interacting with patients. “There are more subtle signs, too, like not touching or coming close to a patient, avoiding eye contact, or showing expressions of discomfort,” Janet Turan adds. “They might seem small, but someone on the receiving end can sense them.”
In rural Alabama and Mississippi, Kempf has found that some physicians don’t even offer HIV tests to their patients because they’re afraid of being ostracized themselves. They don’t want to become known as “the HIV testing doc” and have other patients cancel appointments, she says.
While such cues from health-care workers can have a crucial impact on the way patients view their diseases, they also provide an opening for the UAB researchers, who are training the next generation of physicians and nurses. An effective way to circumvent stigma is to teach these young health professionals to interact with patients in ways that will help them feel comfortable. “Doctors and all health-care providers have a lot of power in their messages,” Hook says. Even small changes can make big differences.
“If a doctor ever comes into a room and says, ‘I’m sorry’ before giving a patient a diagnosis, that’s telling the patient that they have a problem. That maybe the patient should be ashamed,” Hook says. He encourages medical residents never to apologize for a diagnosis, pointing out that this language “provides a permissive role for stigma.”
Feldman has a similar lesson for her medical students: Never call Mr. Smith a schizophrenic; instead, call him a person living with schizophrenia. “That patient is not defined entirely by mental illness,” she explains. The same thing goes for HIV-infected patients, now referred to as “people living with HIV,” Janet Turan adds.
Breaking Discrimination
Fighting stigma’s influence on health outcomes means reducing it at the start, or helping patients receive adequate health care in spite of it. Most researchers agree that education is key to success on both fronts.
“Stigma is categorizing people into pigeonholes and saying, for example, ‘I know a thing or two about people with HIV: They’re immoral, gay, and use drugs,’” says Bulent Turan. “People put others into a category of lesser value with assumptions that may not be remotely true.”
Not only do those assumptions affect current patients, making them feel that they must hide their diagnosis so they’re not lumped into false categories, but they also can prevent others from seeking care in the first place. “It prevents people from getting tested, because they think, ‘I’m not one of those people who does bad things, so I’m not at risk,’” says Janet Turan.
Breaking stereotypes often requires exposure to people who don’t fit them, she adds. “If you get to know someone with a condition personally, you’ll be less likely to discriminate.” With Scott Batey, Ph.D., associate professor of social work in the UAB College of Arts and Sciences, she has spearheaded FRESH (Finding Respect and Ending Stigma around HIV) workshops that bring together health-care workers and HIV patients to talk. The program was designed in Africa but has been adapted for use in Alabama and will soon expand. Initial pilot runs showed that FRESH decreased the stigma felt by patients and increased the empathy felt by health-care workers.
 Jackie Feldman says worries about stigma are a key reason why a large number of people with mental-health issues don't seek treatment.
Jackie Feldman says worries about stigma are a key reason why a large number of people with mental-health issues don't seek treatment.Kempf also has explored telehealth as a way to reach rural, HIV-positive patients in places where they feel safe. The technology could serve as a conduit for care providers and patients to discuss issues they are facing, with the goals of encouraging patients to take medications and providing therapy for depression, she explains.
Seeing the Similarities
Everyone has the power to combat stigma, starting with smashing their own stereotypes about diseases. Again, education and exposure help break down those barriers, Feldman says. “Just reading stories about patients makes you open up,” she notes.
Hook suggests a closer look at facts, which usually hold a few surprises. For example, Hook likes to ask people to guess the average number of sexual partners for a patient in an STD clinic. They rarely answer correctly. In fact, 72 percent of women seeking care for STDs have only one sexual partner, he says. “So when people tell someone with an STD, ‘I think you need fewer sexual partners,’ they have no idea what they’re talking about."
Another way to dial down stigma in communities is to reach out beyond clinics and hospitals, to share the facts with groups likely to cross paths with people struggling with disease symptoms or diagnoses. Feldman says working with religious organizations and schools is a good starting place. “A lot of people turn toward churches, temples, and mosques with their problems,” she says. “And sometimes there is a lack of understanding. We’d like to change that.”
Overall, the message Feldman tries to spread is simple, and one that has lessons far beyond health care. “We’re all much more similar than we are different,” she says.“We have a tendency to hold people at arm’s length and see differences instead of similarities. If we could change that, it would solve so many problems.”

• Learn more about the life-changing research under way in the UAB School of Nursing, School of Public Health, School of Medicine, and College of Arts and Sciences.