 My name is Emani Silva, and this document is for those who are interested in (or currently going through) the Navy’s Health Professions Scholarship Program (HPSP). Your future experience may vary, but I hope this article can answer some of your fundamental questions.
My name is Emani Silva, and this document is for those who are interested in (or currently going through) the Navy’s Health Professions Scholarship Program (HPSP). Your future experience may vary, but I hope this article can answer some of your fundamental questions.
My application experience:
I was first introduced to HPSP through a college teammate who had successfully applied and received the Navy scholarship. Talking with her, I learned about all the great things the Navy had to offer and it sounded awesome to me – especially the part about graduating from medical school with no debt.
I had a semi nontraditional route in that I graduated college a year early but started medical school “on time” – if that makes sense. Typically, students interested in going straight through to medical school start the application process their junior year of undergrad, but because of my timeline, I started my senior year.
I met with my recruiter in June 2017, around the same time I was applying to schools and studying for my MCAT. She was AWESOME and was on top of everything (not always the case for some people so if you choose this route, get used to sending follow-up emails).
Here’s a quick list of things I had to gather for consideration:
-
- Get cleared by MEPS (Military Entrance Processing Station)
- Official college transcripts – 3.2+ undergraduate GPA required
- MCAT scores – 500 MCAT with minimum 124 on each subsection
- 3 letters of recommendation
- An interview with naval physicians – I think I completed 2
- More paperwork
I officially submitted my application in October 2017 and was notified a month later that I had been selected for the Navy HPSP scholarship! A huge weight had been taken off my shoulders. During this time, I continued to interview with medical schools and was accepted to UAB School of Medicine in March 2018. I was later commissioned into the Navy as an ensign (O1) in May the same year.
My timeline since then:
-
- 2018: started first year of medical school
- 2019: ODS in Newport, RI
- 2020: STEP 1 and started third year
- 2021: STEP 2, applied to MODS/ERAS, audition rotations in California and Florida
Why the Navy?
If you choose to go this route, you can apply to all the branches if you really want to – Navy, Army, and Air Force. I was most interested in the Navy program because I grew up close to Annapolis, Maryland, home of the Naval Academy. Navy medicine offers unique opportunities in aviation and undersea medicine. You can also opt to work with the Marines (which is something I am interested in). I also loved the opportunities the Navy offers to deploy on humanitarian missions around the world. Plus, they offer many duty stations in areas near the coast.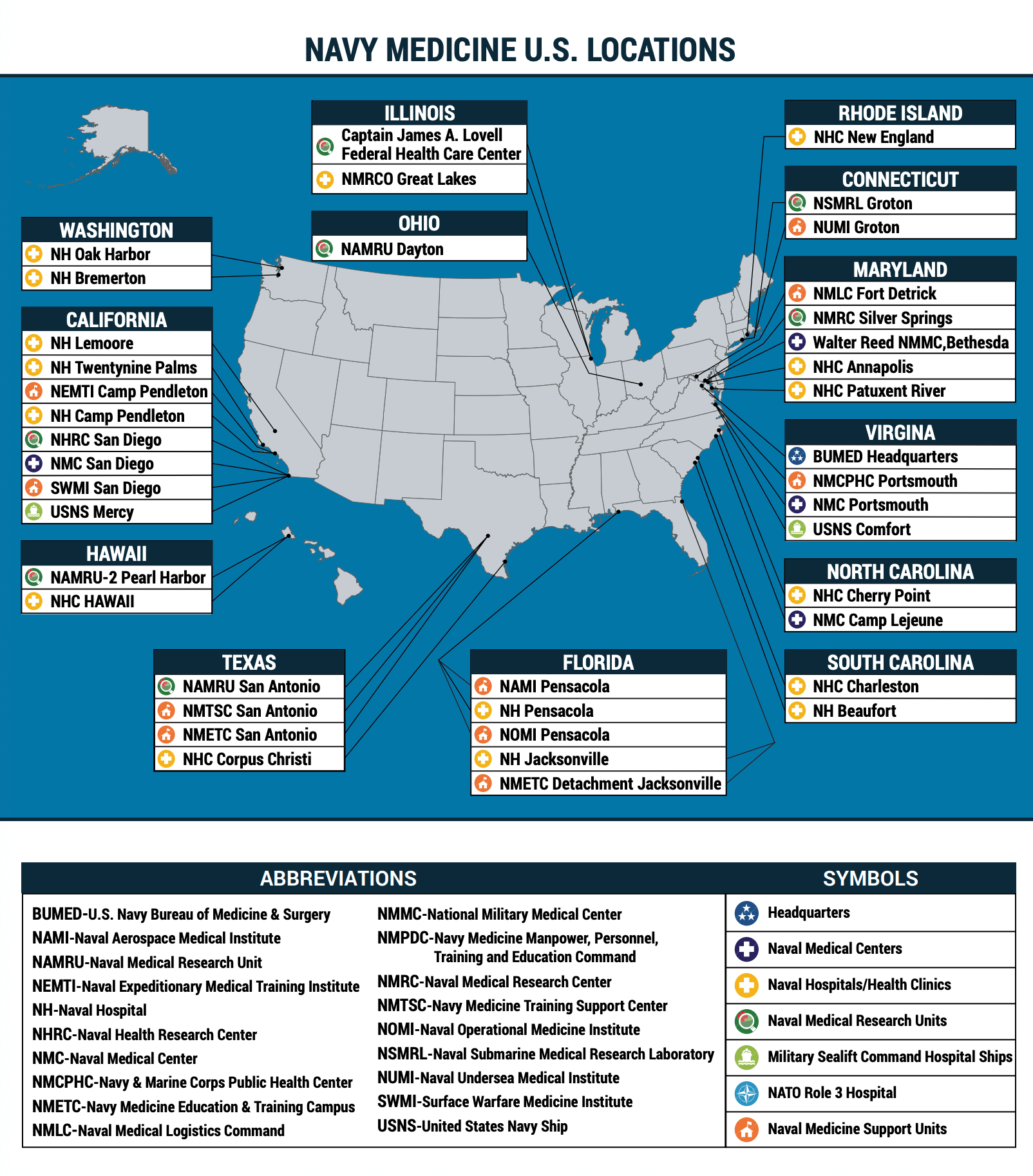 Click to enlarge
Click to enlarge
What does HPSP offer?
HPSP offers full-tuition scholarships, plus a monthly stipend of over $2,300/month and a $20,000 signing bonus in return for a 3-4 year commitment to serve as a naval physician. Future physicians are commissioned as ensigns (O-1) and promoted to lieutenants (O-3) upon graduation.
What are my requirements during medical school?
While in medical school your job is to become the best doctor possible. The office works hard to make sure our service obligations do not interfere with school. Primary obligations to the navy each year include an annual health certification and one, 6-week Active Duty Training (ADT) per year.
What is ADT?
Technically as an HPSP student, we are reservists. As such, we are required to serve 6 weeks of active duty per year. Because our primary responsibility is school, the HPSP office tries to coordinate with us in regards to how we want to spend this time. The most common pathway is listed below:
- Summer between first and second year: Officer Development School
- ODS is in Newport, RI. Training lasts 5 weeks and is typically less intense than boot camp. It is designed to be your first step in development as an officer and will familiarize you with customs, courtesies, and traditions. It is also an opportunity to meet other HPSP students across the country and to get your uniforms situated.
- Summer between second and third year: school orders to study for board exam
- Third and fourth year: away rotations and audition rotations.
- The benefit of doing this while on an ADT is that, in addition to active duty pay, funding for travel, lodging, and food is provided. Where you can travel during these rotations depends on which specialty you are most interested in. As a future Family Medicine physician, my choices included California, Florida, North Carolina, and Washington, DC.
Military Match:
Both civilian and military residencies undergo the match process in which students apply for a limited number of residency programs. The military match occurs in December, whereas the civilian match occurs in March of your application year. As an HPSP student, you are required to apply for the military match, but there are some opportunities to apply to civilian residencies, depending on your specialty. Students can be selected into Navy Active Duty Delay for Specialist (NADDS) program which allows students to complete a civilian residency.
A note like the one listed below will be posted during the spring of your third year. This outlines the number of available residency positions according to specialty and location. Note that only some specialties (ie. Anesthesia, EM, etc) offer NADDS opportunities. Traditionally, approximately 10% of students are authorized for NADDS. “TY” stands for transitional year, which is the most common for those who apply into more specialized residencies including dermatology or radiology. This is like civilian residencies as it is a year that provides a fundamental base of knowledge for interns.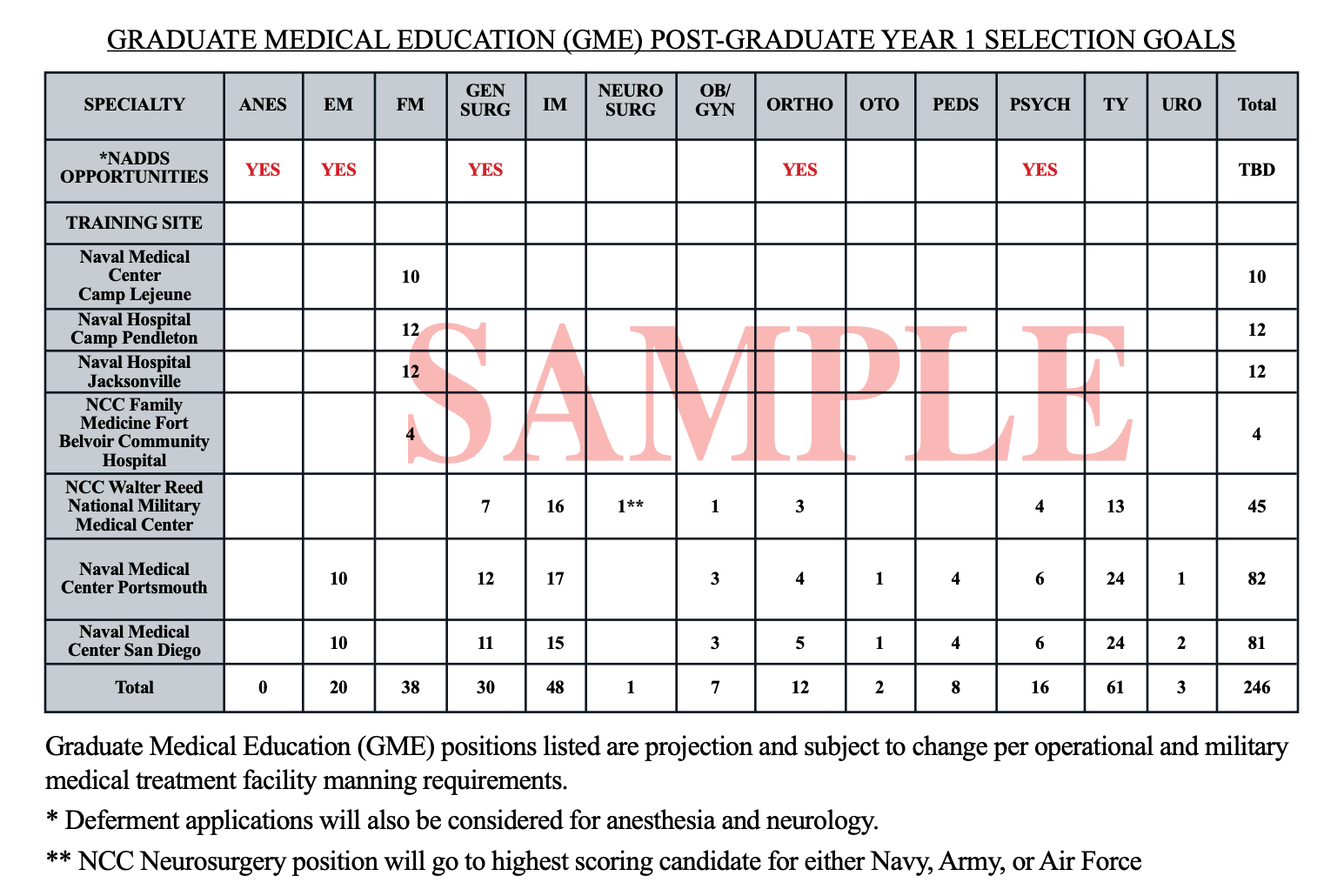 Click to enlarge
Click to enlarge
Military residencies:
Military residencies offer some of the best medical training in the country. In addition, you will receive full officer pay PLUS benefits (ie. basic housing allowance, basic sustenance allowance) that significantly exceed civilian residency pay. If you stay in long enough you also can receive veteran benefits including the Post 9/11 GI bill and healthcare.
When you go into a military residency program there are a few pathways people don’t tend to talk about:
- Straight through residency training: This is like civilian residencies where you complete all years of residency in consecutive order. For example, if you went into Family Medicine, you would complete all 3 years of training then be considered for operational/academic billets.
- Intern year > general medical officer > finish residency: Yes, after applying to residency, you have to apply to stay in the residency program (OR go operational if that’s what you are interested in). People selected for operational medicine after their intern year are typically referred to as General Medical Officers (GMO). These are physicians who have completed their intern year and have a medical license to practice in the U.S. They are typically thought of as general practitioners who can work in undersea/dive, aviation, Marine Corps, or surface warfare communities. They are responsible for first-line trauma management, urgent care, and health maintenance. Additionally, you will have the opportunity to work with and teach corpsmen who can assist you in the medical environment.
- Flight surgeons: receive an additional 6 months of flight school and aviation physiology training to care for pilots and members of the aviation community. You can be assigned to fixed-wing or helicopter units in the Navy or Marines, sea-air rescue units, or the Blue Angels.
- Undersea Medical Officers (UMO): receive radiation health and hyperbaric medicine training in Panama City Beach, FL to become qualified US Navy Divers. UMOs are assigned to diving units including the Navy SEALS, Explosive Ordnance Disposal (EOD), and submarine squadrons. UMOs do NOT deploy with submarines; they oversee the medical care provided by trained Independent Duty Corpsmen (IDC) who deploy with the submarines.
- Fleet Marine Medical Officer (FFMOs): medical experts for the Marine Corps Commanding Officers. They oversee medical readiness and supervision of IDCs, Pas, and Hospital Corpsmen. They provide patient care, patient tracking, and field trauma care and resuscitation. They are expected to meet the Fleet Marine Force (FMF) qualification requirements.
If you have questions about HPSP, please contact medschoolscholarship@uab.edu for more information.