 Patients with Alzheimer’s disease or dementia from traumatic brain injury may resist care efforts from family members, such as taking a bath, taking medicine, routine mouth care, abstaining from alcohol or going to a medical appointment.
Patients with Alzheimer’s disease or dementia from traumatic brain injury may resist care efforts from family members, such as taking a bath, taking medicine, routine mouth care, abstaining from alcohol or going to a medical appointment.
When this resistance is accompanied by agitation, aggression and irritability, it can trigger distress and health issues among family members, reducing their quality of life and increasing the cost of care for the affected person.
Armed with preliminary evidence that professional caregivers can be taught strategies to alter such behavior, University of Alabama at Birmingham researchers are now launching a three-year study to see if family caregivers can benefit from those same strategies.
The hope is that six weeks of personalized coaching, via phone or online, will reduce the burdens felt by the caregivers of family members with dementia.
“We want to know what the family needs are. How do we meet those family needs?” said David Geldmacher, M.D., professor of the UAB Department of Neurology and director of the Division of Memory Disorders and Behavioral Neurology. “Where do they see gaps? What limits their quality of life?”
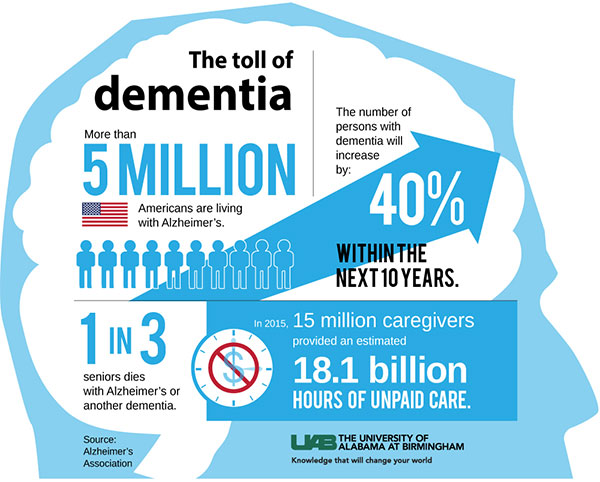
The need to help family caregivers of dementia patients is immense. According to the Alzheimer’s Association, more than 5 million Americans are living with Alzheimer’s, and in 2015, more than 15 million caregivers provided an 18.1 billion hours of unpaid care.
Each family will be trained by Rita Jablonski-Jaudon, Ph.D., associate professor in the UAB School of Nursing and a nurse practitioner in UAB Memory Disorders Clinic, and Vicki Winstead, program manager in the School of Nursing.
Caring for a family member
Jablonski-Jaudon has firsthand experience, as a researcher, clinician and daughter-in-law.
“I cared for my mother-in-law, who had early stage dementia,” she said. “We had to move her from her home to ours. After a particularly rough and humbling week, I remarked to a colleague, ‘I am considered a nursing and research expert in dementia; if I’m struggling, how much harder is this for other caregivers?’”
In nursing home research of older adults with dementia, Jablonski-Jaudon and her staff were able to use specific behavioral techniques to minimize care-resistant behavior.
“We were focused on mouth care, the one activity that consistently triggers resistance to care in persons with dementia,” Jablonski-Jaudon said, adding that those techniques were useful to counter a variety of refusal behaviors.
 Jablonski, GeldmacherIn the current study of family-member caregivers, the UAB team will enroll 50 families of patients with behavioral and psychological symptoms of dementia, and 25 families of patients with traumatic brain injury, or TBI, who have behavioral symptoms that are triggered by caregiver requests. All families will come from patient pools at UAB’s Kirklin Clinic and Spain Rehabilitation Center.
Jablonski, GeldmacherIn the current study of family-member caregivers, the UAB team will enroll 50 families of patients with behavioral and psychological symptoms of dementia, and 25 families of patients with traumatic brain injury, or TBI, who have behavioral symptoms that are triggered by caregiver requests. All families will come from patient pools at UAB’s Kirklin Clinic and Spain Rehabilitation Center.
Family members will be able to watch short videos that cover many of the topics and questions Jablonski-Jaudon has encountered in her outpatient clinics. The videos show techniques to prevent and minimize care-resistant behavior, and family-member caregivers will also receive six, once-a-week coaching sessions, via the GoToMeeting computer app. This will enable face-to-face discussion at convenient times for the families, without the need to travel away from home.
A need to help veterans
The UAB study is funded by a $500,000 grant from the U.S. Department of Defense. The Pentagon is interested in dementia for two reasons, Geldmacher says: Surviving World War II and Korean War veterans are growing ever older, and TBI — a risk factor for dementia — is an important type of injury from the Iraq and Afghanistan wars.
Geldmacher says his team will characterize the nature of the problem for each caregiver family. After Jablonski-Jaudon and Winstead finish their coaching, outcomes will be measured by objective data, such as the number of emergency room visits, and self-reported data, using the standard dementia quality of life surveys. There will also be a long-term follow-up at six, 12 and 18 weeks after the coaching.
“So much is based on an individual’s perceived quality of life,” Geldmacher said. “Something that helps one caregiver family might make another family worse. We anticipate that the study will mostly be families where a child takes care of a parent.”
Geldmacher says he used to give dementia patients periodic exams, and he would usually have to tell the family that the patient was getting worse. That routine was jolted when the son of one patient said, “We know she is getting worse. What can we do?”
That challenge changed Geldmacher’s focus. He began to question how well he was treating the family’s quality of life and how he might better help family caregivers.
At UAB, Geldmacher holds the Patsy W. and Charles A. Collat Endowed Professorship in Neuroscience.
|
“I cared for my mother-in-law, who had early stage dementia… After a particularly rough and humbling week, I remarked to a colleague, ‘I am considered a nursing and research expert in dementia; if I’m struggling, how much harder is this for other caregivers?’” —Rita Jablonski-Jaudon |