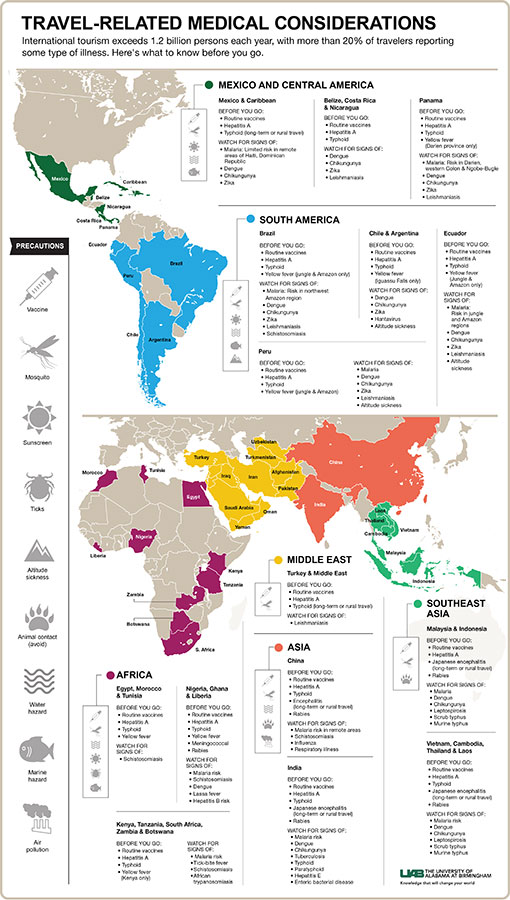
 Click to enlargeInternational tourism exceeds 1.2 billion persons each year, with more than 20 percent of travelers reporting some type of illness. Based on a review article in the New England Journal of Medicine, David Freedman, M.D., founder of the University of Alabama at Birmingham Traveler’s Clinic, recommends international travelers see their health care provider for a pre-travel consultation.
Click to enlargeInternational tourism exceeds 1.2 billion persons each year, with more than 20 percent of travelers reporting some type of illness. Based on a review article in the New England Journal of Medicine, David Freedman, M.D., founder of the University of Alabama at Birmingham Traveler’s Clinic, recommends international travelers see their health care provider for a pre-travel consultation.
“Often people traveling abroad are unsure or unaware of what they should be asking and doing when it comes to their health,” said Freedman, professor in UAB’s Division of Infectious Disease. “Physicians can provide information and interventions during a simple office visit to help reduce illness and disease when traveling. People need the health care knowledge prior to travel to help figure out which of the interventions and education materials apply to their trip.”
Resources are available through the UAB Travelers Health Clinic to help travelers focus on what is needed for their trip.
Pre-travel consultation
A structured medical visit consisting of a risk assessment, in-office interventions, and focused education and safety tips can efficiently identify and address the needed preventive and education to prepare travelers for their trip. The consultation should take place four to six weeks before leaving the United States.
Physicians assess the risk and well-being of the traveler by looking at overall medical history, including medications, disabilities, immune status, immunizations, surgeries, allergies, pregnancy and breastfeeding.
Prior travel experience and the specific itinerary help identify the needed pre-travel interventions and education. Physicians base interventions on the specific regions, season, dates and accommodations of the trip, along with any activities that are planned, especially those for the more adventurous traveler. The traveler’s risk tolerance and financial challenges will also be assessed to determine appropriate interventions.
In-office interventions
During the office visit, there are destination-based interventions and education, such as immunizations, malaria prevention and travelers’ diarrhea, that can help travelers avoid illness and reduce the risks of travel-related health and safety problems.
“The risk of acquiring these diseases is increased when visiting developing countries,” Freedman said. “Taking advantage of these interventions could help save travelers from ruining their trip.”
Physicians will review previous vaccinations along with the traveler’s destination to determine any updates or additional vaccinations needed. The travel consultation is an opportunity to update vaccines with boosters and determine other vaccines needed based on destination. Vaccinations and boosters could include:
- measles-mumps-rubella
- varicella
- influenza
- pneumococcal
- tetanus-diphtheria-acellular pertussis
- hepatitis A
- typhoid
- hepatitis B
- yellow fever
- rabies
- polio
- meningococcal
- Japanese encephalitis
- cholera
- tick-borne encephalitis
Malaria transmission, a life-threatening mosquito-borne infectious disease caused by a parasite, was found in 95 countries and territories last year. Malaria is prominent in areas of Mexico, the Caribbean, South America and Asia, with the highest risk being in central and southern Africa. Mosquitoes that carry malaria are typically night-biters. A standby drug may be prescribed in anticipation of risks based on the area of travel.
Behavioral strategies that can help reduce exposure to malaria are discussed during a travel consultation, and include:
- wear long sleeves and long pants exposing as little skin as possible
- use insect repellent with 30-35 percent DEET or 20 percent picaridin
- treat clothing with permethrin, an insect repellent
- sleep under a permethrin-soaked bed net, specifically if you are not sleeping in a sealed, air-conditioned room in areas of high risk
More than 10 percent of travelers experience travelers’ diarrhea, three or more unformed stools plus at least one accompanying symptom, such as fever, for more than a 24-hour period during travel or seven days after travel.
“Most of the time, travelers’ diarrhea is bacterial, but we have seen an increase in norovirus or rotavirus travelers’ diarrhea,” Freedman said.
Travelers should be cautious about food and water intake, a major cause of travelers’ diarrhea. Education on self-treatment for travelers’ diarrhea consists of oral hydration paired with medications that alleviate symptoms and/or inhibit or reduce secretion. Severe diarrhea may be treated with antibiotics, and prophylaxis may be used for those at a higher risk.
Focused education
Personal protection measures should be discussed during the office visit. More extensive educational materials based on destination help prepare travelers and can provide resources while abroad.
Arthropod-borne illness, such as malaria, dengue, chikungunya, Zika virus, leishmaniasis, rickettsial disease and sleeping sickness, should be discussed along with ways to prevent infection.
High-altitude sickness can occur when travelers ascend, by motor vehicle or airplane, too quickly. When the body does not receive enough oxygen, high-altitude sickness can occur causing a headache, loss of appetite and trouble sleeping. Severe complications include pulmonary or cerebral edema, or swelling or pressure in the lungs or brain.
| Travelers should stay hydrated, perform leg exercises while on flights lasting more than four hours and use compressions socks to help circulate blood. |
“High-altitude sickness can be prevented by ascending gradually,” Freedman said. “Physicians can also prescribe acetazolamide, a diuretic or ‘water pill.’ It is important to consult your physician to determine the best plan of action when climbing to high altitudes.”
The lack of mobility during travel could cause travelers’ thrombosis, or blood clots in the leg veins. Travelers should stay hydrated, perform leg exercises while on flights lasting more than four hours and use compressions socks to help circulate blood. Those at a high risk of thrombosis should administer a prophylaxis just before departure and 24 hours later. Aspirin has not been proved to benefit travelers.
Other travel-related illness to consider talking with a physician about include respiratory infection, tuberculosis, blood-borne and sexually transmitted infections, rabies and animal-related illness, skin conditions and wounds, transportation-associated illnesses, and motor vehicle injury, as well as activity-based illness from swimming, such as water exposure and marine hazards.
“I recommend taking a medical kit and medical care when traveling abroad,” Freedman said. “This can include a personal health kit, information about medical facilities in the area you are traveling in and evacuation insurance.”