UAB Fertility Advances Bring Help and Hope
By Julie Hall Bosché
Sometimes it takes a little science to help fulfill a dream. At least that’s what it often feels like for people who turn to UAB’s Division of Reproductive Endocrinology and Infertility for answers, help, and hope.
 Success stories: G. Wright Bates, director of UAB's Division of Reproductive Endocrinology and Infertility (left, with patient Staci Cornelius and her daughter, Hannah), says that UAB's success rate for in vitro fertilization has more than doubled in less than 10 years and now often exceeds 50 percent in a month. Now more of those dreams are coming true. In less than 10 years, UAB’s success rate for in vitro fertilization (IVF) has more than doubled. Division director G. Wright Bates, M.D., credits much of the success to refinements in IVF techniques. “We have come a long way in treatment cycles,” he says. “Back in 2002, less than one in four women with a good prognosis got pregnant within a month. Now we often exceed 50 percent in a month with IVF.” He adds that increased awareness of infertility issues—and more widespread information on potential solutions—also has helped educate the public and encouraged more patients to learn about their options.
Success stories: G. Wright Bates, director of UAB's Division of Reproductive Endocrinology and Infertility (left, with patient Staci Cornelius and her daughter, Hannah), says that UAB's success rate for in vitro fertilization has more than doubled in less than 10 years and now often exceeds 50 percent in a month. Now more of those dreams are coming true. In less than 10 years, UAB’s success rate for in vitro fertilization (IVF) has more than doubled. Division director G. Wright Bates, M.D., credits much of the success to refinements in IVF techniques. “We have come a long way in treatment cycles,” he says. “Back in 2002, less than one in four women with a good prognosis got pregnant within a month. Now we often exceed 50 percent in a month with IVF.” He adds that increased awareness of infertility issues—and more widespread information on potential solutions—also has helped educate the public and encouraged more patients to learn about their options.
Increasing the Chances
Today, the division, which provides individualized care to both women and men, continues to investigate new advances in fertility treatment that will increase the chances of conceiving and carrying healthy babies. One avenue of research is the multicenter PCOS-II Trial, sponsored by the National Institutes of Health (NIH), which is testing two oral medications, clomiphene citrate (Clomid) and letrozole (Femara), to determine which is the most effective in inducing ovulation and enhancing fertility in women who have irregular cycles, don’t ovulate regularly, or exhibit signs of hormone imbalance.
|
WATCH: Infertility: 35 is the new 25 Wright Bates discusses the latest science in fertility treatment in this video presentation. |
“We’re thrilled to be part of this group,” Bates says. “There is no other center in the Southeast participating, and we think it’s a great way for us to improve our treatment options, and better serve the women of Alabama.”
The trial covers basic fertility testing for both women and men and provides four months of treatment. Patients interested in enrolling in the trial can call study coordinator Susan Mason at (205) 801-8207 for more information and a phone screening.
Another revolutionary development, Bates says, is pre-implantation genetic screening, which examines embryos for disease and potential developmental problems. “This doesn’t mean designer babies, or choosing hair color and eye color,” Bates explains. “We’re talking about ensuring a normal chromosomal number and avoiding major developmental issues to enhance the chances of producing a normal, healthy offspring.”
Bates is quick to underscore the division’s emphasis on healthy pregnancies. UAB is committed to avoiding high-order multiples—triplets or more—that can pose a threat to both the woman and the fetuses, he says.
Fertility After Cancer
Beyond assisting couples who are struggling to conceive, Bates and his colleague Janet McLaren, M.D., are focusing on ways to help cancer patients who have concerns about their future reproductive capabilities. UAB is participating in the National Physician Cooperative and Oncofertility Consortium, an NIH program working to develop techniques to improve the reproductive prospects of people who have undergone treatments such as chemotherapy or radiation that can be detrimental to fertility.
“As treatments for cancer have improved, survival has become more commonplace. People are going on to live full lives, and for many of them, that includes having children,” Bates says.
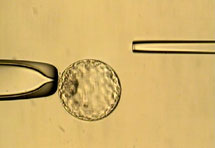 |
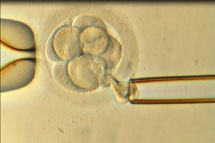 Pre-implantation genetic screening allows UAB physicians to examine embryos for chromosomal abnormalities and major developmental issues. Pre-implantation genetic screening allows UAB physicians to examine embryos for chromosomal abnormalities and major developmental issues. |
A very successful solution for these patients, he notes, is fertility restoration, in which donated eggs or sperm allow couples who are infertile from treatment to experience pregnancy and parenthood. And both women and men can benefit from a variety of fertility preservation techniques, Bates says, including banking sperm, eggs, embryos, or an ovary before cancer treatment begins.
The newest and most experimental of these techniques is ovarian tissue cryopreservation, in which a woman’s ovary is harvested and frozen. Following successful cancer treatment, the frozen tissue is transplanted back to the remaining ovary in the woman’s body. While only about two dozen pregnancies worldwide have resulted from this technique, Bates says that it is particularly promising for women and young girls for whom reproduction may not be a priority now, but who may want children in the future.
Bates adds that the majority of patients who have sought information regarding fertility preservation prior to cancer treatment have chosen to not pursue fertility preservation or use traditional IVF with embryo freezing, with only a small number pursuing egg or ovarian tissue banking. However, it is very important to note that simply having the options discussed and their questions addressed may allay some common fears about cancer treatment, he explains. “We want to help people go from surviving cancer to surviving parenthood,” Bates says.
More Information
UAB Division of Reproductive Endocrinology and Infertility
Patient Kelly Key talks about her experience with fertility treatment at UAB in this video
