By Gail Allyn Short

Cardiac rehabilitation offers patients with heart disease customized plans to tackle lifestyle factors that affect heart health.
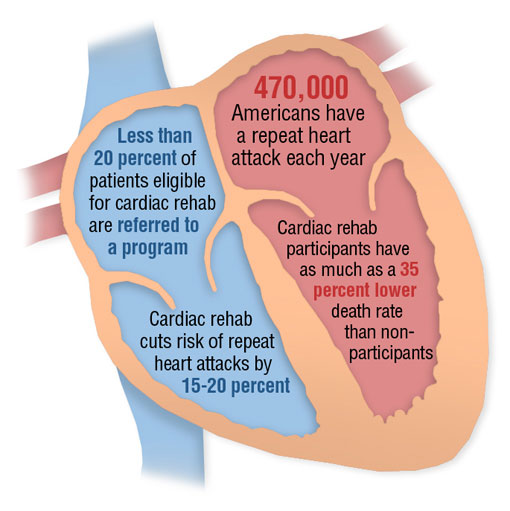
This year, an estimated 785,000 people will experience their first heart attack, according to the American Heart Association. During that same period, some 470,000 people, who have already had one or more heart attacks, will have another. But an intervention program known as cardiac rehabilitation could help reduce both of those sobering figures.
Health professionals working with cardiac rehabilitation develop individualized plans for cardiology patients that target specific problems such as poor diet, stress, smoking, lack of exercise, and other lifestyle factors that affect heart health.
UAB cardiologist Vera Bittner, M.D., medical director of the Coronary Care Unit and the UAB Cardiac Rehabilitation Program, recently reported that, in an analysis of data taken from the Medicare database, cardiac rehabilitation lowered the death rate among participating patients by as much as 35 percent compared to non-participants with similar heart problems.
(Article continues beneath the illustration)
Here’s what you need to know:
1. Many patients with heart problems can benefit
“Cardiac rehabilitation is for the person who already has heart disease,” says Bittner. “This includes patients with stable angina, those who have had a heart attack or who have had a cardiac procedure such as angioplasty/stenting, heart bypass surgery, or other open heart surgeries.” Patients diagnosed with congestive heart failure also benefit from the program, Bittner says, but this indication is currently not covered by Medicare.
The age of the patient can vary, says Bittner. “We’ve had patients who were teenagers as well as people who were in their 90s, so there really is no age limit. Instead of looking at age, we consider whether a patient has a medical condition that would benefit from this course of treatment.”
2. How it works
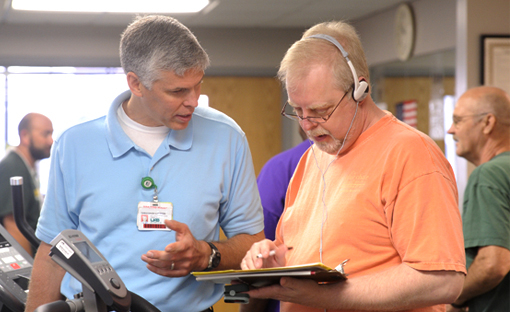
Patients entering the program first receive a thorough health assessment of symptoms, medications, diet, exercise habits, and lifestyle, Bittner says. The information helps to shape an individualized treatment plan for each patient that is directed by physicians and administered by a team of professionals—nurses, exercise physiologists, dietitians, diabetes educators, pharmacists, and psychologists.
Most patients are put on a medically supervised regimen of aerobic exercise and resistance training to tone muscles and improve balance. Each exercise session lasts about an hour. “If they have led a sedentary lifestyle,” says Bittner, “we’ll explore different ways that they can incorporate more activities into their day-to-day routine.”
Besides exercise, patients may meet with dieticians to establish heart-healthy eating habits. Patients also attend education classes, led by physicians, to learn more about their illnesses and medications. Additional services include counseling to help patients quit smoking and manage stress and depression that can result from having a heart attack, Bittner says. The average cardiac rehabilitation is 12 weeks, depending on a patient’s condition.
(Article continues beneath the slideshow)
3. What are the benefits?
Besides reducing mortality, some studies have shown that cardiac rehabilitation cuts the risk of recurrent heart attacks by 15 to 20 percent, says Bittner. “We also have good data showing that it improves blood pressure, cholesterol levels, exercise capacity, symptoms, depression, and general sense of well being,” she says. Cardiac rehabilitation can also lead to weight loss and fewer hospitalizations.
4. Are there risks?
There are very few people who would not benefit from cardiac rehabilitation, says Bittner. The exercise regimens, for example, are moderated depending on the age and condition of the patient, she says. “We emphasize a gradual buildup from their current level of physical capacity to what is optimal for them. So that may vary depending on whether it’s a 25-year-old who has just had valve surgery or an 85-year-old who is recovering from a heart attack. We don’t take anyone who has been terribly sedentary and put them in something that looks like boot camp.” Nonetheless, the program is not recommended for patients with severe and uncontrolled heart rhythm issues or those with severe pulmonary hypertension.
5. How do you get into a program?
“Patients are generally identified for cardiac rehabilitation after they are admitted to cardiac inpatient services,” says Bittner. They may also get a referral from their own doctors. Unfortunately, Bittner says, less than 20 percent of patients eligible for cardiac rehabilitation are referred to a program. She encourages patients who think they might benefit to bring it up with their doctors.
“We shouldn’t think of cardiac rehabilitation as something that’s optional and medications and procedures as life saving,” says Bittner. “We need to change that mindset given the data that we have on the improvement of mortality so that people will think it just as essential to participate in cardiac rehabilitation as it would be to take an aspirin every day along with their cholesterol and blood pressure medicine.”
For more information about UAB CardioPulmonary Rehabilitation Services, call UAB HealthFinder at 1-800-822-8816 or visit this site.