Carolyn Walsh was traveling on Interstate 459 in Birmingham when she began to feel “off.” She was fighting to stay awake at the wheel, experiencing bouts of severe drowsiness. Before she could pull over, Walsh was in a car accident. Besides a scare, all parties involved were unharmed.
But the accident was a wake-up call. Walsh sought answers to her dangerous drowsiness and received a surprise diagnosis by her general physician: type 2 diabetes. She began medication but had difficulty managing her disease. She finally visited an endocrinologist, who put her on insulin injections immediately, which she notes was the best thing she ever did for her health.
However, Walsh found herself at UAB Hospital-Highlands a few years later when she woke up feeling nauseated, fatigued, breathless, and weak. The team at Highlands quickly recognized that Walsh was facing a potential deadly condition that required immediate treatment: diabetic ketoacidosis. Her cells were not converting blood sugar into energy, so her liver began to break down fat for fuel. A UAB endocrinologist was able to provide a personalized diagnosis: latent autoimmune diabetes in adults, not type 2 as she originally thought.
“Seeing someone who specializes in your specific condition is a smart step in managing your health,” Walsh says. “Having a specialist provide me with the specific latent autoimmune diabetes diagnosis was a game-changer in taking care of myself.”
In 2017, Walsh started receiving nutrition counseling from Amy Warriner, M.D., a professor in the UAB Division of Endocrinology, Diabetes, and Metabolism, which Walsh notes was a critical step in her journey with diabetes.
Now, Walsh, communications director for the UAB Department of Medicine, feels that she is at a manageable place in her disease with her care team’s help. “My connection is very personal. I received lifesaving care here at UAB, and the follow-up transformed how I live with diabetes,” Walsh says. “At every step of the way, people have been rooting for me to be healthy. When I show up in clinic and in the nutrition counseling sessions, they behave like a community of support for me. Absolutely, I’ve got skin in this game, and they do, too. I hope we win the fight together.”
Walsh is one of the approximately 14 percent of adult Alabamians living with diagnosed diabetes. Each year, almost 30,000 adults in Alabama are diagnosed with diabetes, and it is estimated another 120,000 Alabamians have undiagnosed diabetes. The state ranks third in percentage of adults with diabetes and is considered part of the “Diabetes Belt,” a region of the southern United States where people are more likely to have type 2 diabetes than people in other parts of the country.
Given these statistics, UAB and the UAB Marnix E. Heersink School of Medicine have made a priority of understanding diabetes and developing new and better approaches to diabetes care and prevention. The following highlights just a few of the innovative programs housed across the Heersink School of Medicine.
A Milestone in Excellence
2023 marks the 15th anniversary of the UAB Comprehensive Diabetes Center (UCDC), the result of a collaborative effort between UAB, Children’s of Alabama, and supporters in the Birmingham community. The UCDC is composed of over 200 faculty members from 10 different schools and numerous departments, a reflection of the complexity of the disease and the center’s “all hands on deck” approach to understanding the biological mechanisms at work in diabetes and developing new and improved therapies, with the ultimate goal of developing cures.
The UCDC was established in 2008 with a mission to perform cutting-edge research, train future diabetes professionals, and develop novel treatment approaches. The UCDC also serves as the umbrella for various research programs and awards, including the prestigious P30 Diabetes Research Center, U01 Human Islet Research Network grants from the National Institutes of Health (NIH), and several research core facilities.
One of the UCDC’s most promising avenues of research involves a drug called verapamil that was originally developed as a blood pressure medication. Identifying oral verapamil as a potential type 1 diabetes drug was the discovery of UCDC Director Anath Shalev, M.D., a professor in the Division of Endocrinology, Diabetes, and Metabolism and holder of the Nancy R. and Eugene C. Gwaltney Family Endowed Chair in Juvenile Diabetes Research.
This finding stemmed from more than two decades of Shalev’s research into a gene in pancreatic islets called TXNIP. TXNIP is elevated in diabetes and toxic to islets, and verapamil helps bring TXNIP levels back to normal. In 2012, Shalev’s UAB research lab reported that verapamil completely reversed diabetes in animal models, and in 2015 she announced plans to
test the effects of the drug in a human clinical trial.
Type 1 diabetes is an autoimmune disease that causes loss of pancreatic beta cells, which produce insulin. To replace that, patients must take insulin by shots or pump and are at risk
of dangerous low blood sugar events. There is currently no oral treatment for the disease. In 2018, Shalev and colleagues reported the benefits of verapamil in a one-year clinical trial of type 1 diabetes patients, finding that oral administration of verapamil enabled patients to produce higher levels of their own insulin, thus limiting their need for injected insulin to regulate blood sugar levels.
In March 2022, Shalev’s team reported in the journal Nature Communications that use of verapamil to treat type 1 diabetes continues to show benefits beyond one year. Patients taking the medication not only required less daily insulin two years after first diagnosis of the disease, but also showed evidence of surprising normalization of multiple immunological markers.
The beneficial effects of verapamil have now also been independently validated in children with T1D and a large multi-center clinical follow-up trial is ongoing in Europe. A large clinical study from China also demonstrated the benefits of verapamil in the context of type 2 diabetes. In addition, the findings have paved the way for the development of a novel, even more potent and specific TXNIP inhibitor drug and the spin-off of a UAB start-up company (TIXiMED, Inc.) to help move this discovery into patients.
“In humans with type 1 diabetes, even a small amount of preserved insulin production—as opposed to higher insulin requirements—has been shown to be associated with improved outcomes and could help improve quality of life and lower the high costs associated with insulin use,” Shalev says. “The fact that these beneficial verapamil effects persist for two years provides additional support for its potential usefulness for long-term treatment.”
Understanding Diabetes in Minority Youth
The prevalence of type 2 diabetes in youth is increasing in the U.S., primarily among minorities, with Black and Hispanic youth showing the greatest increase. Neither the reason for the increase nor the mechanism underlying the disproportionate risk in minority youth is known.
UAB researchers received more than $3.7 million from the NIH to study the increasing prevalence of diabetes in youth as part of a nationwide consortium. Barbara Gower, Ph.D., interim chair and professor in the Department of Nutrition Sciences in the UAB School of Health Professions, and Ambika Ashraf, M.D., director of the Division of Pediatric Endocrinology and Diabetes at UAB and Children’s of Alabama, are leading the UAB site. UAB is one of 15 institutions selected to participate.
“Our research aims to predict which youth are at greatest risk for developing type 2 diabetes, as well as identify the determinants of progression to type 2 diabetes,” Ashraf says. Preventing the progression to type 2 diabetes is essential. “The knowledge gained from this study would allow us to develop targeted prevention approaches to treat at-risk children,” says Gower.
Over the course of the project, which will end in November 2027, researchers hope to enroll 1,500-3,000 youth who are at risk for diabetes. The main objective of the study is to identify factors that predict conversion to type 2.
All participants will be nondiabetic, but at risk, at the time of recruitment and baseline testing. The team of researchers will assess body composition, continuous glucose monitoring, beta-cell function, insulin sensitivity, diet, physical activity, pubertal progression, psycho-social factors, the intra-uterine environment, and other factors that may affect risk for type 2 diabetes.

Preventing Diabetic Blindness
The leading cause of blindness in American adults is diabetic retinopathy, progressive damage to blood vessels in the light-sensitive tissue at the back of the eye. Yet the source of this damage appears to lie in the belly—mainly a leaky small intestine that weakens the barrier between gut bacteria and the blood system, according to a study published in the journal Circulation Research.
The research blood from human subjects with Type 1 diabetes and a mouse model of Type 1 diabetes were used to explore mechanisms underlying diabetic retinopathy. The results show a way to possibly prevent, or even reverse, the eye damage.
It is known that Type 1 diabetes dysregulates the systemic renin-angiotensin system, or RAS. RAS is a system of hormones and enzymes that regulates blood pressure and other metabolic changes. Besides systemic RAS, there are also local RAS networks that act in diverse tissues. One key RAS enzyme is ACE2, or angiotensin-converting enzyme 2.
The loss of ACE2 in diabetes activates the vasodeleterious RAS axis and lessens the vasoprotective RAS axis. Intriguingly, in a mouse model of Type 1 diabetes, feeding mice with a modified gut bacterial strain of Lactobacillus paracasei, which was engineered to produce human ACE2, protects the mice against diabetic retinopathy progression. Finally, lack of ACE2 in the gut was known to increase gut permeability and systemic inflammation.
The human studies compared people with Type 1 diabetes versus controls. The subjects with Type 1 diabetes were further stratified into three groups: no diabetic retinopathy, non-proliferative diabetic retinopathy, and the more serious disease called proliferative diabetic retinopathy. By measuring levels of certain immune cells and biomarkers in the blood, including gut microbial antigens, the researchers found that human subjects with retinopathy had a dysregulated systemic RAS and profound gut permeability defects that activated components of both the adaptive and innate immune response. Furthermore, increases in the severity of diabetic retinopathy were found to correlate with increased levels of gut permeability biomarkers and a gut microbial antigen. This included increased levels of angiotensin II, the RAS hormone that activates the vasodeleterious RAS axis.
“To our knowledge, this study represents the first time gut barrier disruption has been implicated in the pathogenesis of diabetic retinopathy and also directly links gut leakage with retinopathy severity in human subjects with Type 1 diabetes,” says Maria Grant, M.D., leader of the research team and a professor in the Department of Ophthalmology and Visual Sciences.
Forging New Approaches
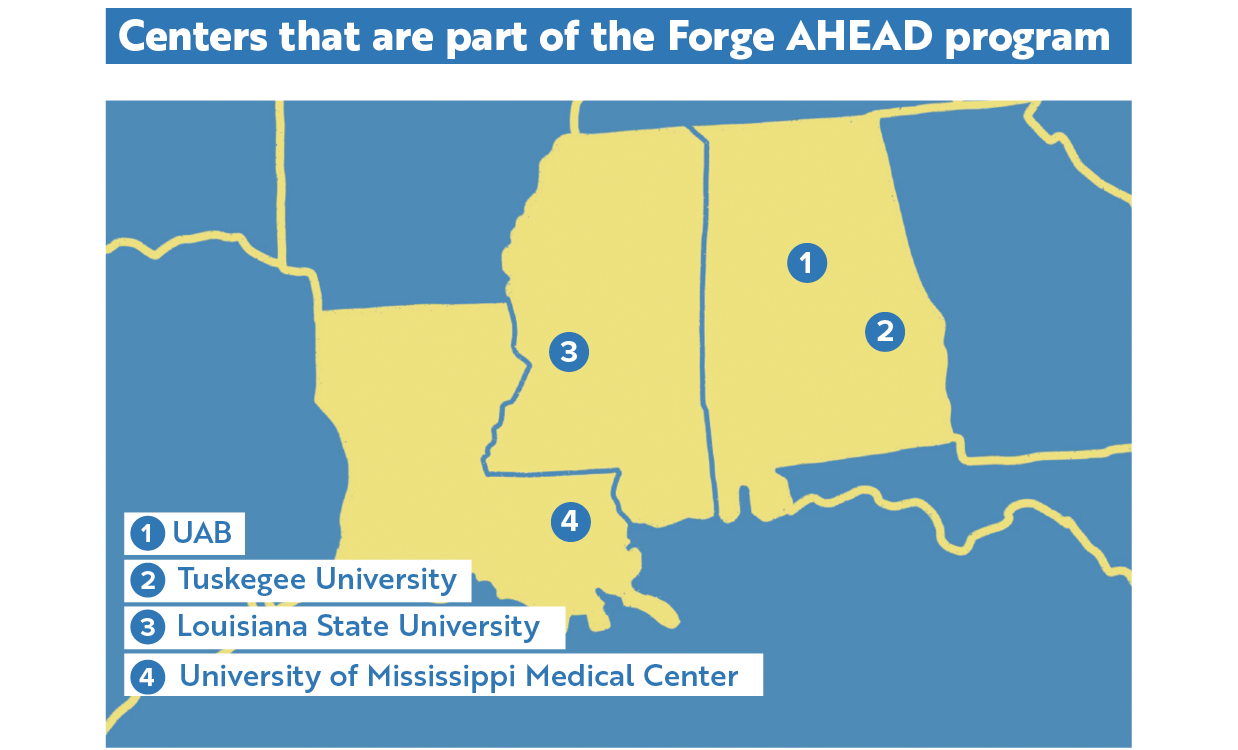
The Forge AHEAD (Advancing Health Equity Across the Deep South) Center was established in 2021 as a collaboration between UAB, Tuskegee University, Louisiana State University System’s Pennington Biomedical Research Center (PBRC), and the University of Mississippi Medical Center (UMMC). The center is funded by the National Institute on Minority Health and Health Disparities with a mission to promote health equity and reduce the burden of cardiometabolic diseases, including diabetes, obesity, and hypertension, among Black Americans and low-income populations in Alabama, Mississippi, and Louisiana.
At UAB, Forge AHEAD is led by Andrea Cherrington, M.D., MPH, professor and interim director of the Division of Preventive Medicine, along with Gareth Dutton, Ph.D., a professor in the Division of Preventive Medicine, and Orlando Gutierrez, M.D., professor and director of the Division of Nephrology. According to Cherrington, the center is made up of an administrative core, a community engagement core that houses a community advisory board and a growing community coalition, and an investigator development core.
The center also supports three R01 level projects. One project that focuses on obesity and diabetes is located in New Orleans and is led by Peter Katzmarzyk, Ph.D., of the PBRC. This clinical study is using patient portals and health coaching to try to improve outcomes. Another project is a community-based study in Alabama and Mississippi that focuses on a combination of peer coaching and community gardens to address obesity, pre-diabetes, and hypertension; the Alabama study is led by Monica Baskin, Ph.D., an adjunct professor in the UAB Division of Preventive Medicine. The third project is led by Tapan Mehta, Ph.D., vice chair for research in the UAB Department of Family and Community Medicine. It is an optimization trial that is recruiting patients in Alabama and Mississippi with poorly controlled diabetes, existing cardiovascular disease, and high levels of social vulnerability. The study is looking at a combination of interventions to improve outcomes that include remote patient monitoring, digital health coaching, and a food delivery service.
“The center has several goals,” says Cherrington. “One is to advance the science around cardiometabolic disparities through these projects. Another big component of the center is focused on growing and diversifying the pool of investigators focused on health equity and health disparities in our region. So we have a scholars program that includes pilot funding for projects for junior investigators, as well as a curriculum that helps provide our investigators with information and skills needed for this kind of work.”
Welcoming Renowned Researchers
In July 2023, the Heersink School of Medicine and the UCDC welcomed renowned clinician-scientists Rita Basu, M.D., and Ananda Basu, M.D., as professors into the Division of Endocrinology, Diabetes, and Metabolism as well as senior scientists in the UCDC and Hugh Kaul Precision Medicine Institute (PMI). In addition, Rita serves as a chair of the UAB Institutional Review Board (IRB) as well as the inaugural medical director of the UAB Office of the IRB, and Ananda serves as the director of the UAB Diabetes Technology Programs.
“As world-renowned researchers, Drs. Rita and Ananda Basu each bring unique and invaluable knowledge and expertise in using sophisticated tracer studies to study type 1 and type 2 diabetes in humans,” says Shalev.
“We are very much looking forward to the many collaborative opportunities that Rita’s and Ananda’s recruitment creates across the center, with the Hugh Kaul Precision Medicine Institute, and across campus.”
After over two decades at the Mayo Clinic, Rita was recruited to the University of Virginia (UVA) in 2017, where she served as a professor in the Division of Endocrinology and the clinical education director of the Center of Diabetes Technology.
Besides serving as a chair of the Mayo Clinic IRB for more than 10 years, Rita was also the associate medical director of the Human Research Protection Program and was responsible for the accreditation of the Mayo health system IRB. At the University of Virginia, Rita was again the IRB chair and made significant improvements and reforms.
Rita serves as the principal investigator on several NIH- and industry-funded projects, including one that seeks to understand insulin resistance in humans that is currently in its 40th year of continuous funding. She has also been an active researcher in the field of non-alcoholic fatty liver disease and has co-authored management guidelines for endocrinologists.
Rita’s work has produced around 175 peer-reviewed publications in scientific journals and has presented more than 150 abstracts in national and International Scientific meetings. She serves on the editorial board of the prestigious American Journal of Physiology as well as the high-impact American Diabetes Association journal Diabetes Care.
Ananda held several leadership positions spanning almost three decades at the Mayo Clinic, and was an endowed professor of medicine as well as a clinical investigator at UVA.
He serves as the principal investigator/co-investigator on multiple NIH projects. His primary research focus is to better understand glucose and glucagon physiology in type 1 diabetes with the ultimate goal to help develop the next generation artificial endocrine pancreas that recreates as closely as possible a truly functional islet. His work also aims to develop a closed loop glucagon infusion therapy to prevent hypoglycemia in patients with post bariatric surgery hypoglycemia syndrome.
As a dedicated clinician, Ananda established a Transplant Endocrine, a Cardio-Metabolic Clinic, and a Diabetes Technology Clinic at the Mayo Clinic. He also led the Mayo Clinic’s Hospital Diabetes Management team for more than a decade while establishing protocols and standardizing care of hyperglycemic hospitalized patients, and dramatically reduced diabetes-related sentinel events during his tenure.
At UVA Health, he set up a similar multi-disciplinary, Diabetes Technology Clinical program to facilitate the use of continuous glucose monitors and closed loop systems for individuals with type 1 diabetes.
Ananda has authored close to 200 peer-reviewed publications in scientific journals and presented more than 150 scientific abstracts in national and International scientific meetings. He has also served on the editorial board of Diabetes Care and as an associate editor of the Diabetes Technology and Therapeutics journal.
Ananda and Rita Basu are world experts in the development of innovative isotope modeling techniques to study whole body human metabolism and physiology. Both are members of the American Diabetes Association, The Endocrine Society, and the American Physiological Society. Division of Endocrinology, Diabetes, and Metabolism Director Fernando Ovalle, M.D., is pleased to have the Basus become part of the division’s clinical research efforts.
“We could not be more excited to have Drs. Ananda and Rita Basu join our growing division,” he says. “I know that Andy will provide outstanding care to his patients and that both Andy and Rita will continue to advance clinical diabetes research at UAB.”
-By Emma Shepard, Jeff Hansen, Caroline Newman, and Jane Longshore
 From left to right: Barbara Gower, Ph.D.,
Ambika Ashraf, M.D., Maria Grant, M.D., Andrea Cherrington, M.D., MPH,
Gareth Dutton, Ph.D., Orlando Gutierrez, M.D., Monica Baskin, Ph.D., Tapan Mehta, Ph.D., Rita Basu, M.D., Ananda Basu, M.D.
From left to right: Barbara Gower, Ph.D.,
Ambika Ashraf, M.D., Maria Grant, M.D., Andrea Cherrington, M.D., MPH,
Gareth Dutton, Ph.D., Orlando Gutierrez, M.D., Monica Baskin, Ph.D., Tapan Mehta, Ph.D., Rita Basu, M.D., Ananda Basu, M.D.