Media contact: Anna Jones
 Pulsed-field ablation disrupts the cellular membranes of vein tissue, irreversibly preventing those membranes from conducting electricity. This protects the heart from the rapid impulses which can cause atrial fibrillation.
Pulsed-field ablation disrupts the cellular membranes of vein tissue, irreversibly preventing those membranes from conducting electricity. This protects the heart from the rapid impulses which can cause atrial fibrillation.
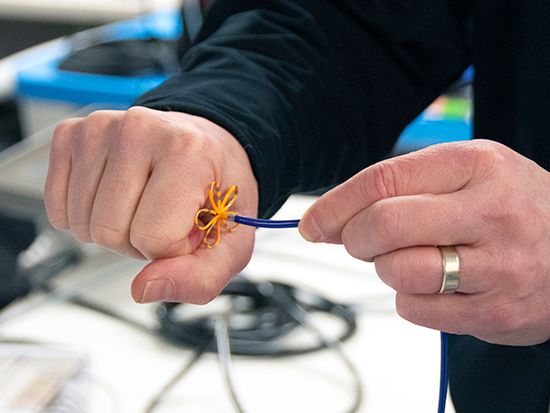
Photography: Andy CurrieElectrophysiologists at the University of Alabama at Birmingham Cardiovascular Institute are among the first in the nation to use pulsed-field ablation to treat atrial fibrillation. According to Tom McElderry, M.D., an associate professor of medicine in the UAB Division of Cardiovascular Disease, this novel therapy uses fast, high-energy electrical pulses to ablate pulmonary veins and atrial tissue safely and effectively.
“Pulmonary veins can fire impulses rapidly,” McElderry said. “Those impulses are conducted down the vein, into the heart, and can knock it into atrial fibrillation, an irregular and rapid heart rhythm. The condition affects nearly 6 million people in America.”
Pulsed-field ablation disrupts the cellular membranes of the tissue, irreversibly preventing those membranes from conducting electricity. This protects the heart from the rapid impulses that can cause atrial fibrillation.
“You can imagine that the veins are like a copper pipe,” McElderry said. “Fluid could run inside the pipe, but electricity could also run outside the pipe. So, as we go in and ablate around the vein, it is like putting a rubber washer between a copper pipe and another metal structure. We have electrically isolated the vein.”
The advantage of this new technology is the ability to tune the waveform to target specific tissues while sparing structures like nerves and smooth muscle of the esophagus. This targeting helps prevent some of the worst possible complications, including phrenic nerve injury and left atrial esophageal fistula. McElderry has worked on developing pulsed-field ablation for more than a decade.
“I got involved with this technology almost 10 years ago,” McElderry said. “We first used this energy source in an open-chest surgical procedure. We then did some cadaver work in Seattle. From there, we did some work in Bordeaux, France, and then did the first human cases in Paraguay. Treatment at UAB is the culmination of all that work.”
McElderry is a leader in the development and delivery of the pulsed-field ablation procedure, alongside the entire team, who is trained to use the novel technology for patients in the UAB Heart and Vascular Center — one of the largest and most advanced cardiovascular clinical facilities in the Southeast.
Given the successes of this therapy, UAB Medicine’s Cardiovascular Institute aims to improve and expand its uses in the future, with the potential to look outside the pulmonary veins, at targets that are difficult to treat and address with current technology.