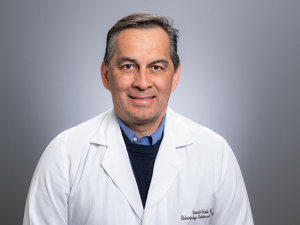
Rebecca Rampe, Psy.D., works with patients to build “other templates that are more authentic to them as adults and to create a new relationship with the self." At parties, when talk turns to work, Rebecca Rampe, Psy.D., has learned to stay quiet. Rampe specializes in helping adults who have endured horrific abuse, neglect or other harsh adversity in childhood, or who have been shattered by the sudden, violent, complex death of a loved one, often a child.
Rebecca Rampe, Psy.D., works with patients to build “other templates that are more authentic to them as adults and to create a new relationship with the self." At parties, when talk turns to work, Rebecca Rampe, Psy.D., has learned to stay quiet. Rampe specializes in helping adults who have endured horrific abuse, neglect or other harsh adversity in childhood, or who have been shattered by the sudden, violent, complex death of a loved one, often a child.
“I don’t often tell people what I do,” said Rampe, a clinical psychologist and assistant professor in the Department of Psychiatry and Behavioral Neurobiology. “People don’t want to hear about it or talk about it.” But her willingness to talk about these topics is exactly why she ended up where she is.
“I became a psychologist due to my own experience of developmental trauma, which has driven me to create healing spaces for adults who have had difficult childhood experiences,” Rampe said. After her father died from an overdose in 2019, she became interested in the topic of traumatic grief, as well. She sought out specialized training to help patients grieving in the wake of sudden, violent or complex deaths.
This fall, Rampe launched the UAB Developmental Trauma and Traumatic Grief Clinic, which provides specialized support and therapeutic approaches not available anywhere else in Alabama. Within a few weeks, the clinic was fully booked. This is not a surprise. Statistics indicate that both developmental trauma and the conditions that often lead to traumatic grief are increasing.
In 2017, researchers estimated that up to 19 percent of American youths have experienced physical abuse by a caregiver and one in 10 has witnessed serious violence between caregivers. Childhood emotional abuse is even more widespread, reported by an estimated 36 percent of the adult population, with emotional neglect in childhood reported by 18 percent of adults. Meanwhile, traumatic losses have soared recently. In the past two years, rates of murder, suicide and fatal drug overdoses each reached all-time highs.
Developmental trauma: Creating a new relationship with the self
Rampe, who joined UAB in 2021 after more than a decade at the University of North Carolina Wilmington, says that treatment works for most people — and there are few practitioners in Alabama specializing in this area.
Adult repercussions of childhood trauma
“Childhood experiences can still be impacting us in the present in ways we may not be fully aware of or able to change alone," Rampe said. This may include difficulties with:
- managing emotions
- self-regulation
- relationships
- body awareness
- self-compassion
“Childhood experiences can still be impacting us in the present in ways we may not be fully aware of or able to change alone,” Rampe said. “This may be difficulties with managing emotions, self-regulation, relationships, body awareness and self-compassion. Childhood trauma often leads to engaging in adaptive habits for the time that no longer serve us outside of that childhood setting.”
Rampe works with patients to build “other templates that are more authentic to them as adults and to create a new relationship with the self,” she said. Developmental trauma is often associated with post-traumatic stress disorder. But “most developmental trauma does not manifest as symptoms of PTSD in adulthood,” Rampe said, and most of the patients she sees do not have a PTSD diagnosis.
Rampe said her approach is highly integrative, meaning “I am a huge advocate of making the treatment fit the person, rather than the other way around.” So Rampe and the students she trains in her clinic have to know “quite a few therapy models,” she said. “We have an emphasis on emotion-focused, compassion-focused and body-based approaches that are formed into a treatment plan to meet the unique needs of the person.”
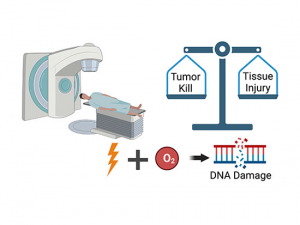
Rampe’s clinic is the only one in Alabama to offer services through the Neurosequential Model of Therapeutics™, or NMT, developed by Bruce Perry, M.D., Ph.D., of Northwestern University. “Early-life trauma acts on core regulatory networks in the brain” that are involved in distributing dopamine, serotonin and norepinephrine, Rampe said. “It disturbs brain stem development and can make sensory regulation difficult.”
Because the brain stem reacts rapidly, before the brain’s executive regions can weigh in, “our body will tell us first” how we should react, Rampe said. “If it was not safe when you were a child, if nobody cared or nobody was around, that can alter how you understand sensations or nervous system states as you move through the world.”
Some patients live in a permanent state of survival response — the basic fight, flight or freeze options that are maintained by an underlying feeling of being unsafe. For other patients, there may be difficulty relating to others. “If you have sensory overload, a massage therapist may help you get to the point where you can tolerate touch,” Rampe said. “NMT is very creative and holistic in how it looks at therapeutic approaches. We admit that some of this stuff is so deep-rooted that we can’t talk ourselves out of it. Talk only includes the cortex; if you are dysregulated, it is harder to have access to these states.”
Traumatic grief: Complicated and misunderstood
Rampe’s interest in traumatic grief began with her father’s fatal overdose. “People say really mean, crappy things” at times like these, Rampe said. “There is victim blaming, saying they did it to themselves, that they didn’t care about other people because they struggled with addiction.”
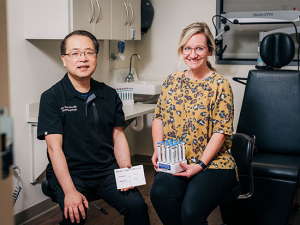
Training students
The UAB Developmental Trauma and Traumatic Grief Clinic is staffed by Rampe as well as advanced graduate students from UAB’s Ph.D. in medical/clinical psychology program and interns in UAB’s American Psychological Association-accredited doctoral internship program. Learn more about UAB psychology graduate programs here.
After her father’s death, Rampe sought out training in the Compassionate Bereavement Care Model, developed by Joanne Cacciatore, Ph.D., including advanced training for traumatic grief. She is the only provider in Alabama with this training.
Many of Rampe’s patients experiencing traumatic grief are parents who have lost a child, but they may also be coping with other sudden losses of individuals or pets. “Loss due to traumatic grief is often complicated and misunderstood by providers and the public,” she said. “It can be shocking in its intensity and often overwhelms the person’s ability to cope. I am a parent of two young kids, and that is the worst thing that I could imagine.” But she also knows “some parents who have had a child die and no one would work with them.”
The latest version of the DSM, the standard manual for psychiatric diagnoses, lists criteria for “prolonged grief disorder” that include grieving that lasts longer than six months. “Parents who have a child die are more likely to be diagnosed with prolonged grief disorder,” Rampe said. “Parents get diagnosed with a disorder because they are grieving. Death is the one shared human experience we will have; but we don’t allow people to talk about that without a timeline, as if a person should be over it in two months or three months.”
And that arbitrary timeline has consequences, Rampe says. “Fifty percent of parents who have a child die are prescribed a medication within a week,” she said “I understand the impulse behind that. We don’t handle distress well. We want them functioning. But people complain that they can’t feel their emotions and connections when they are on these medications. And that love doesn’t go away when the person dies; it is an unfair expectation that we can integrate that into our lives in a specific time frame.”
Expanding influence across the state
Although the Developmental Trauma and Traumatic Grief Clinic is fully booked, Rampe says it will introduce prevention programming and community education opportunities next year.
The clinic is staffed by Rampe, advanced graduate students from UAB’s Ph.D. in clinical and medical psychology program, and interns in UAB’s American Psychological Association-accredited doctoral internship program. Appointments take place mainly through telemedicine in order to make the services more widely available.
After working with Rampe and her patients, do the students and interns she trains at UAB (and before that, at UNCW) ever want to stick with it? “Yes, they often want to work with this population in longer-term settings,” Rampe said. In the future, she said, she would “love to open up this clinical training option to graduate students across the state.”
Rampe added that she is grateful to Rachel Fargason, M.D., Patrick Linton Professor in the Department of Psychiatry and Behavioral Neurobiology, “for supporting this new clinic endeavor.”
Related article
UAB researchers share insight on PTSD and upcoming research Rampe and Merida Grant, Ph.D., director of the Trauma-Related Disorders Clinic in the Department of Psychiatry and Behavioral Neurobiology, explain more about trauma disorders and research ongoing in the department.