|
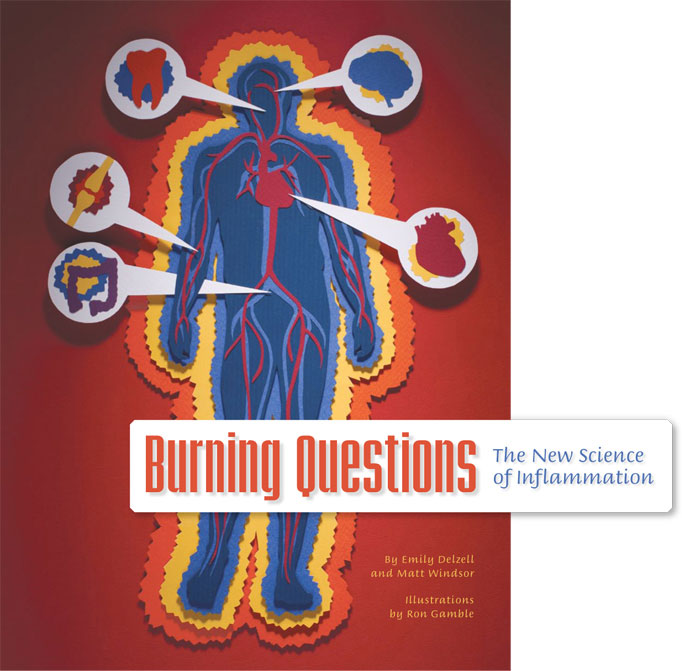
INFLAMMATION IS EMERGING as one of the medical archvillains of the 21st century, a chemical axis of evil that works in mysterious ways to destabilize our health. It contributes to nearly every major health problem, including heart attacks, cancer, obesity, diabetes, and Alzheimer’s disease. Imagine you cut your finger—while flipping through this magazine, for instance. Even as you wince in pain, your immune system is on the case. Mast cells stationed near the cut leap into action. They fire off chemical signals called cytokines to call in reinforcements, and release blood vessel-dilating histamine to speed the arriving warriors into battle. Blood vessels also become more porous, which allows immune cells to slip out of the bloodstream and reach the injury site. (This process also brings the redness and swelling that are two chief hallmarks of inflammation.) |
|
|
|
More macrophages appear, and natural killer cells, which are armed with cell-shredding granules, also join the battle. When the invaders are subdued, platelets and other healing factors close the wound and repair any remaining damage. In addition to cuts, the same process of acute inflammation can cope with viral infections, burns, and other threats. Normally, the inflammatory reaction to invasion is swift and contained. But sometimes, for reasons that are still unclear, the inflammatory cascade never reaches its designated finale. The process remains active, albeit at a lower level, for months or years. This chronic inflammation was once dismissed as little more than a nuisance. But it is becoming increasingly clear that chronic inflammation represents a dangerous imbalance—in fact, it shares much in common with autoimmune disorders, in which the body mistakenly targets normal tissue for destruction. 
Civil WarUAB rheumatologist Kenneth G. Saag, M.D., M.Sc., specializes in the dark side of inflammation. He leads an active research program to evaluate new treatments for complex autoimmune conditions such as rheumatoid arthritis. “When the immune system and its inflammatory processes go awry and attack the body they are designed to protect, the result is autoimmunity,” Saag says. In rheumatoid arthritis (RA), antibodies move into the linings between bones, causing chronic inflammation that produces swelling and excess fluid along with stiffness, pain, and redness. Constant inflammation wears down cartilage and can damage surrounding tendons, ligaments, and muscles. Over time, this ongoing damage can painfully twist and deform joints. Chronic ConflictThe trigger that sets off RA is still unknown, but the disease can clearly reach beyond the joints and nearby tissues to affect the eyes, the lining of the lungs, and the heart. “This persistent inflammation is a well-established, independent risk factor for both cardiovascular conditions and bone loss,” Saag says. In the past decade, researchers have discovered that the inflammation-disease connection isn’t restricted to autoimmunity. Mounting evidence connects chronic inflammation with increased risk for everything from Alzheimer’s disease and diabetes to migraines and cancer. Click the link below to learn more, as UAB researchers report from the front lines of one of the hottest topics in medicine.
|
 The first to arrive are neighboring macrophages (“large eaters”), which begin to destroy invading bacteria and your own damaged cells. Then come the neutrophils, which swallow bacteria and damaged tissue and dispatch them by secreting a lethal dose of superoxide.
The first to arrive are neighboring macrophages (“large eaters”), which begin to destroy invading bacteria and your own damaged cells. Then come the neutrophils, which swallow bacteria and damaged tissue and dispatch them by secreting a lethal dose of superoxide.