By Emily Delzell
|
|
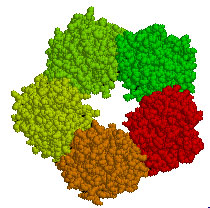
A computer model of C-reactive protein |
UAB immunologist Alexander J. Szalai, Ph.D., is collaborating with other UAB scientists in multiple disciplines to understand the varied actions of C-reactive protein (CRP), ranging from its damaging role in heart disease to its potential protective effects in autoimmune disorders such as systemic lupus erythematosus and multiple sclerosis (MS).
Although too much CRP in the blood may indeed fuel heart disease, the work of Szalai and his colleagues suggests too little may contribute to the risk and development of lupus and MS.
“You wouldn’t want to have zero CRP in the body,” Szalai says. “For example, compared with their normal or ‘wild type’ counterparts, in mice we’ve genetically engineered to express human CRP, we’ve seen delayed onset of both lupus and MS. CRP appears to be acting in a protective role in these autoimmune conditions. Learning how CRP operates to effect this protection could suggest new drug targets.”
Szalai and colleagues also are investigating a newly proposed role for CRP—one that is played out independently of inflammation, its traditional partner in immune defense. “There is evidence that CRP may also help regulate homeostasis, the stable, constant state the body’s internal systems need to maintain life,” he says.
The body strives constantly for homeostasis by producing chemical checks and balances that keep its many internal systems, including core temperature and blood sugar level, constant despite an ever-changing environment. Eat a slice of rich chocolate cake, for example, and the body releases a flood of insulin to take up excess glucose, or sugar, from the blood. When insulin control fails, diabetes is the result.
“We propose that CRP acts as a regulator of homeostasis by maintaining and fine tuning insulin control,” Szalai says. Specifically he and his colleges think CRP regulates the release of insulin degrading enzyme (IDE), which helps clear insulin from the blood when its job is done and may also play a role in breaking it down inside cells.
“Chronically high or low CRP levels appear to cause disease,” he says. “Clinical evidence supports our theory. Trials show that lowering CRP significantly reduces heart disease, but increased the diabetes rate by 25 percent.”
Szalai and colleagues have begun a study using transgenic mice to test his theory of CRP as a homeostatic regulator. Their long-term goal is providing information to advance development of drugs that target the physiological pathway on which CRP, IDE, and insulin converge.
“CRP and IDE are also linked to other metabolic diseases and to Alzheimer's disease, so better understanding of these important components could lead to therapies for some of our society’s most prevalent and destructive illnesses,” he says.