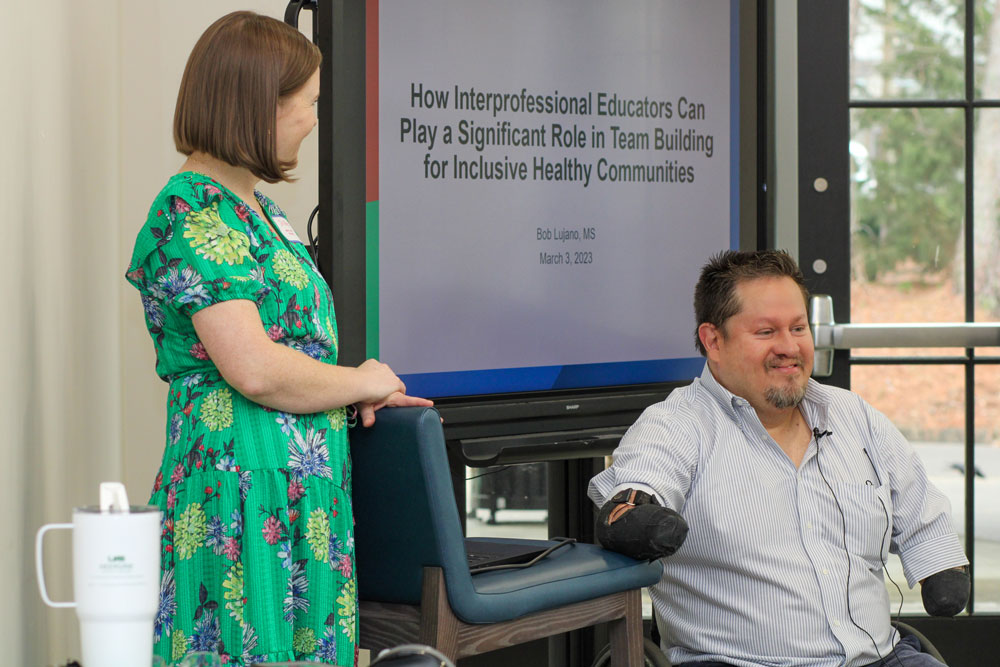
Speaking to students and faculty from several programs at UAB, Samford University and Cahaba Medical Care, Bob Lujano, MS, shared his experience as a someone with a disability, and focused on how primary care providers can make the medical world – and the world in general – more accessible and inclusive.
Lujano, an employee with Birmingham’s Lakeshore Foundation for more than 20 years, is an international public speaker. In his talks, he covers topics related to disability and inclusion such as independence, faith, leadership, competitive sports, and the benefits of a healthy and active lifestyle. Currently, Lujano is an inclusion specialist with the National Center on Health, Physical Activity and Disability (NCHPAD), headquartered at the Lakeshore Foundation, which doubles as an official Olympic and Paralympic Training site. Lujano is a member of the Lakeshore Demolition wheelchair rugby team and a veteran of the US Paralympic Rugby Team. He took home the bronze medal at the 2004 Olympic Games in Athens, Greece.
Lujano addressed attendees of the Comprehensive Urban Underserved and Rural Experience program (CU2RE) Friday, at their “Teams Retreat: Together Everyone Achieves More.” The Department of Family and Community Medicine’s CU2RE program aims to increase the number of physicians practicing primary care in rural and urban underserved areas. In addition to CU2RE medical students, students and faculty from the UAB Department of Nutrition Sciences, Samford University School of Pharmacy, Samford University School of Health Professions, Speech Language Pathology and Physical Therapy, and Cahaba Medical Care’s Social Work Program were also present.

Students in each of these programs will eventually enter a workforce where they will work alongside multiple health professions to provide high quality, patient-centered care. Creating space for students to learn cross-discipline collaboration in primary care settings is one of the CU2RE program’s priorities. This approach affords students the opportunity to communicate and learn from their peers so that, together, they can address patient needs holistically, especially complex cases where social determinants of health impede health equity. Through collaborative leadership, primary care teams can effectively coordinate care and heighten patient experience by extending greater assistance to individuals with a disability. More so, teaching students how to work in interprofessional teams will advance their understanding towards scope of practice of other team members. It will also lend greater insight into how they can collectively support a patient’s medical and non-medical needs, and how to improve patient outcomes by more effectively managing pre-existing conditions and preventing new ones.
During his talk, Lujano discussed how his medical team helped him in the decades after he lost his limbs at age 9, when he contracted a rare form of meningitis called meningococcemia. Lujano will always remember Physical Therapist Debbie Short, who consistently sought creative ways to get him to practice walking with prosthetic limbs. Short helped young Lujano get used to his prosthetics in six short weeks, before he went back to school.
“You will have a great responsibility. You may affect people’s lives that you do not even know, by something subtle that you say or do, or maybe something that you don’t say, even just being there,” he told the students. After all, “I am talking about a therapist who was part of my life over 30 years ago.”

As they navigate spaces built without their needs in mind, Lujano also talked about challenges people with disabilities may face within the health care system and in the world at large.
About one in four, or 61 million U.S. adults, has a disability. Unfortunately, many are more susceptible to stroke, diabetes, heart attack, obesity and other health issues. This is, in part, due to the barriers people with disabilities often face while trying to participate in physical activities, exercise programs, or when going to gyms to work out, Lujano said. He remembers, during P.E., his instructor told him to play chess while other kids in his class played sports. Lujano says it was an isolating experience. By high school, he was determined to be involved in sports. He has stayed active ever since and has worked to make recreational activities more accessible to people with disabilities. Lujano also encouraged clinics to adopt simple changes, like having wheelchair-accessible scales for patients to get an accurate weight.
“If you have a lack of access to recreation, or if you are not able to know your weight,” Lujano said. “There could be a lot of [undetected] underlying health conditions.”
In another example, when Lujano had a heart attack in 2017, he had to lift and balance himself on an x-ray table taller than he was. The wheelchair rugby player was perfectly capable of accomplishing this feat, but he believes others with similar disabilities might not have been able to do it.
These are all examples of ableism – intentional or unintentional discrimination against people with disabilities. Today, Lujano said, he most often encounters ableism in subtle ways, such as when a restaurant server asks his wife for his food order when he is sitting directly beside her, or when someone addresses a disability as a tragedy.
“Disability is the best thing that ever happened to me, and there are benefits to me having a disability,” he said. “Not everyone with disability feels that way, and it is fine, but it is about claiming who you are.”

He encouraged current and future medical providers in the room to think about the language they use, like saying, “people with disabilities,” instead of a “disabled person” and to notice how patients with disabilities describe themselves. Some may want to name their specific disability or otherwise self-identify.
He also pushed them to pay attention to, and call out, barriers to access. Lujano grouped those barriers into three categories: architecture, attitudes and programs.
Held at The Bell Center, a center for children who are at risk for developmental delays, Lujano pointed out how accessible he found the retreat’s location— wide hallways and doorways, bathrooms accessible for wheelchairs, ramps into the building and parking close to the entrance.
By actively planning to have people with disabilities participate, and by showing people with disabilities in marketing materials, he said programs can be made more accessible.
Barriers caused by attitudes, said Lujano, are the most prevalent.
“Sometimes, when people see me come through the door, they don’t know what to do with me,” he said. Lujano reminded students they control their attitudes; he told them they could all be proactive in creating a welcoming environment for patients with disabilities. In addition to being mindful of their language, Lujano encouraged those in attendance to be aware of barriers patients face and not to be afraid to speak up on their patients’ behalf.
Two quotes he used in his presentation captured these takeaways:
“There is a difference between ‘All are welcome here’ and ‘This was created with you in mind.’" – Anonymous
“Our lives begin to end the day we stay silent about things that matter.” -- Dr. Martin Luther King, Jr.
This program is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $7 million with 10% financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government.