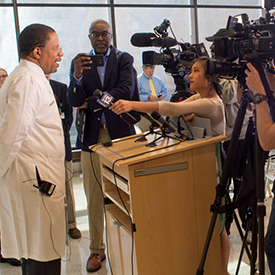
 Selwyn Vickers, dean of the School of Medicine, speaks to members of the media at a press conference in March announcing the Alabama Genomic Health Initiative. Imagine editing a book with about 6 billion characters subdivided into words, paragraphs, and chapters, and poring over each letter and space to ensure every character is in its proper place and there are no periods where a comma should sit. That book would be nearly 625 times longer than the current Guinness World Record holder for longest book, A la recherche du temps perdu by French author Marcel Proust, which comes in at a shade over 9.6 million characters across 13 volumes.
Selwyn Vickers, dean of the School of Medicine, speaks to members of the media at a press conference in March announcing the Alabama Genomic Health Initiative. Imagine editing a book with about 6 billion characters subdivided into words, paragraphs, and chapters, and poring over each letter and space to ensure every character is in its proper place and there are no periods where a comma should sit. That book would be nearly 625 times longer than the current Guinness World Record holder for longest book, A la recherche du temps perdu by French author Marcel Proust, which comes in at a shade over 9.6 million characters across 13 volumes.
That is what it takes to sequence and analyze a person’s entire genomic sequence, which is why Bruce Korf, M.D., Ph.D., the chair of the UAB Department of Genetics and the Wayne H. and Sara Crews Finley Chair of Medical Genetics, uses the analogy when describing the genomic analysis and interpretation that will become available, free of charge, to a group of Alabama residents thanks to the Alabama Genomic Health Initiative (AGHI).
Future Medicine
“Since the Human Genome Project was completed in 2003, we’ve learned a tremendous amount about the roles of genes in disease,” says Korf. “This project will result in immediate health benefits to some participants. In the long term, it will help address chronic disease and rising health care costs in the state. It will also position Alabama at the forefront of 21st century medicine.”
A collaboration between the UAB School of Medicine and Huntsville-based HudsonAlpha Institute for Biotechnology, and initially funded by a $2 million appropriation from the Alabama Legislature to UAB, the AGHI will recruit a diverse group of participants from every county in Alabama to receive genomic sequencing. In the first year, the initiative plans to recruit 2,000 people who will provide a DNA sample from a simple blood draw. Over a five-year period, the goal is to increase participation to at least 10,000 people.
“Our goal is to develop a representative cross sample of Alabama residents, broadly characteristic of ethnic, racial, and socioeconomic groups throughout the state,” says Matthew Might, Ph.D., director of the UAB Hugh Kaul Personalized Medicine Institute and co-director, along with Korf, of the AGHI.
The ethical, legal, and social issues surrounding such a project are complex, which is why the AGHI includes a bioethics working group to ensure the highest ethical standards. Bioethicists—one from HudsonAlpha, one from Tuskegee University, and one from UAB—are reviewing all plans and procedures to ensure that appropriate safeguards and protections are in place and to guide the initiative on matters such as privacy, security, and informed consent.
The AGHI is also creating a DNA biobank for research that will impact health and medicine in Alabama and around the world. “This database will be an unparalleled tool for understanding the health risks across different demographics in the state,” says Might. “Researchers working on finding cures for diseases will have the resources to identify genetic factors that predispose individuals to rare or common disorders, with the hope of developing new approaches to prevention, diagnosis, and treatment.”
Unlocking Secrets
The AGHI will initially recruit participants at UAB in Birmingham and later at UAB clinical operations in Huntsville, Montgomery, and Selma. The initiative will eventually expand to other sites in Alabama. Korf says he anticipates the majority of participates will be either healthy or undergoing treatment for one or more conditions not recognized to have a genetic cause. This group’s blood samples will undergo a genotyping array test, which assesses 650,000 identified genomic biomarkers for variants in 59 “actionable genes.” The American College of Medical Genetics and Genomics (ACMG) has identified a set of 59 genes as contributing to disease where there is an established intervention to improve outcomes. “Perhaps the best-known genes on the list are BRCA1 and BRCA2, which are associated with a genetic risk of breast and ovarian cancers,” Korf says. “We will begin with this ACMG list, but we may add to it over time.”
Participants testing positive for one of the 59 actionable genes will receive genetic counseling to interpret the results. Their primary medical providers will also be informed with the permission of the participant. The doctors will then refer their patients to seek appropriate prevention strategies or proper treatment. “The number of individuals likely to get a positive report will be small, maybe 1 to 3 percent, but the results will be life-changing and possibly lifesaving,” Korf says. “There is also a multiplying effect. If one person discovers they are at genetic risk for a disease, then they can relay that information to others in their family. It allows family members to take appropriate action as well.”
A smaller group of AGHI participants will have a recognized genetic issue of undetermined origin. These patients will likely have undergone a “diagnostic odyssey,” moving from specialist to specialist in an unsuccessful quest to identify their mysterious malady. For each person in this group, experts will analyze all 22,000 genes and 6 billion base pairs of DNA, a process called whole genome sequencing which will be conducted at HudsonAlpha, to try to uncover a gene variant that offers a clue to the disease. These results will be shared with the patient and his or her primary medical provider. Participants will also be linked to appropriate medical care, which could include UAB’s Undiagnosed Diseases Program.
“We hope to provide an answer to about 25 to 33 percent of these patients,” says Korf. “We want to tell them, if we can, what the cause of their condition is and, even more important, how we can help them manage or treat it.”
A New Era for Health
The AGHI lays a strong foundation for greater access to precision medicine for Alabamians through its research and clinical components, according to Selwyn M. Vickers, M.D., senior vice president for medicine and dean of the School of Medicine. “It will allow the groundwork to be laid for hopefully everybody in this state to benefit from precision medicine as it evolves and as our knowledge grows,” he says.
Korf agrees this initiative makes precision medicine more accessible to Alabamians. He also notes another benefit to genomic testing: savings in time and money. “A single investment in sequencing can sometimes save many times the cost in unproductive consults and tests.”
By Ryan Broussard