 Earlier research suggests that the use of low-dose atropine drops plays a role in slowing the progression of myopia in children. However, new research co-led by experts in the UAB School of Optometry shows that may not be the case.
Earlier research suggests that the use of low-dose atropine drops plays a role in slowing the progression of myopia in children. However, new research co-led by experts in the UAB School of Optometry shows that may not be the case.
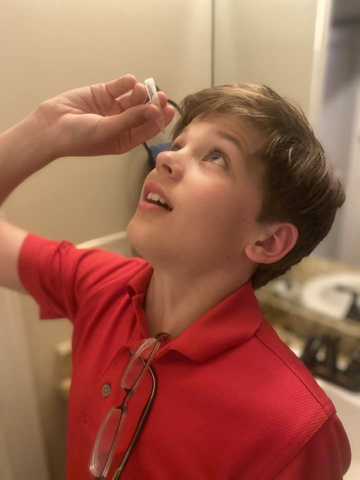
Photo provided by Katherine Weise.It is predicted that, by 2030, some 39 million people in the United States will have myopia, or nearsightedness, according to the National Eye Institute. Earlier research suggests that the use of low-dose atropine drops plays a role in slowing the progression of myopia in children living in Asian countries. However, new research from the University of Alabama at Birmingham found that the use of low-dose atropine eye drops was no better than placebo drops at slowing myopia progression and elongation of the eyes of a diverse group of children living in the United States.
Prior to this research, recent trials conducted primarily in East Asia showed a benefit from .01 percent atropine in slowing myopia. The randomized controlled trial, conducted by the Pediatric Eye Disease Investigator Group and funded by the NEI, studied the use of low-dose atropine drops over the course of two years in children with myopia. Stronger concentrations of atropine drops have been used by eye doctors for years to slow myopia progression, and while these higher doses have proved to be effective, such doses cause light sensitivity and blurry vision. Therefore, researchers are studying lower concentrations of atropine that have been shown to have fewer side effects.
“The different response to atropine in our U.S.-based study compared to East Asian studies may reflect racial differences in how children with myopia respond to low-dose atropine,” said Katherine Weise, O.D., a professor in the School of Optometry and co-lead researcher. “Children in the U.S. may need a different dose of atropine to be able to see a response.”
For the study, 187 children ages 5 to 12 years with low to moderate bilateral myopia were randomly assigned to use nightly low-dose atropine (125 children) or placebo (62 children) eyedrops for two years. Study participants, their parents and the eye care providers were masked to the group assignments. Patient care was provided at 12 study center sites throughout the United States, including UAB. After the treatment period, there were no significant differences between the groups in the degree of myopia compared with baseline or significant differences in axial length when compared with baseline measurements.
Weise reports that 95 percent of the children who began the study at one of the 12 sites across the nation completed the study. At UAB, 100 percent of the children involved in the study completed the study requirements —the most among the 12 centers — with 60 percent of UAB’s participants representing underrepresented minority populations.
“This type of dedication and rigor in research by our very diverse group of trailblazing kids helped us better understand a potential need to shift our focus from this concentration of atropine eye drops in U.S. kids in our work toward understanding nearsightedness better,” Weise said.
Weise says more research is needed to better understand the differences in the myopic eye among different races and ethnicities in order to better tailor treatment options for patients with myopia.
“It was an honor to provide national leadership with Michael Repka, M.D., of Johns Hopkins University for this important study,” Weise said. “I’m also proud of the 25 local kids in the UAB area who were part of this study. These important study results will be read worldwide and further advance the treatment of myopia in children.”
PEDIG is a collaborative network of pediatric ophthalmologists and pediatric optometrists dedicated to conducting multi-center trials on eye disorders that affect children. The trial was funded by NEI grants EY11751, EY18810 and EY23198. The ClinicalTrials.gov identifier is NCT03334253. To read the full study in JAMA Ophthalmology, click here.