Which Test Is Best for Breast Cancer?
By Lisa C. Bailey
 For more than 30 years, breast cancer screening has meant mammography. But how does the traditional test rate against newly developed technologies—particularly breast MRI and molecular breast imaging (MBI)? UAB radiologist Heidi Umphrey, M.D., compares the three exams:
For more than 30 years, breast cancer screening has meant mammography. But how does the traditional test rate against newly developed technologies—particularly breast MRI and molecular breast imaging (MBI)? UAB radiologist Heidi Umphrey, M.D., compares the three exams:
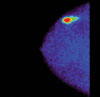
Mammography
Advantages: Mammography is quick, accurate, readily available, and cost-effective, Umphrey says. Recent studies have shown that digital mammography, in which images are viewed on a computer rather than on film, improves accuracy in women under 50 and those with dense breast tissue. Umphrey notes that all patients at UAB receive digital mammography.
Caveats: It involves X rays, which means women receive radiation. But Umphrey says the low dose used is not considered a source of long-term harm. Women with larger breasts and those under 50 with dense breast tissue sometimes need additional views.
Breast MRI
 Advantages: Breast MRI involves no radiation; instead, patients lie on their stomachs in a traditional MRI machine, with their breasts suspended below the table. The test is more sensitive than mammography and is especially useful for women at high risk for breast cancer.
Advantages: Breast MRI involves no radiation; instead, patients lie on their stomachs in a traditional MRI machine, with their breasts suspended below the table. The test is more sensitive than mammography and is especially useful for women at high risk for breast cancer.
Caveats: That high sensitivity increases the number of false-positive reports, which could lead to additional biopsies, Umphrey says. The tests can take up to an hour, and the cost is significantly higher than mammography. In addition, the exam requires an intravenous dose of contrast solution; Umphrey notes that there is a small risk of anaphylactic reaction to the contrast material.
Molecular Breast Imaging (MBI)
 Advantages: Several similar tests fall under the MBI heading; in all of them, women receive an injection of a radioactive solution that accumulates in cancerous cells more than normal cells. Then the women stand or sit with breasts slightly compressed while a scanner images them. Small studies have suggested that MBI can detect up to three times as many cancers in women with dense breast tissue and that it produces fewer false-positive results.
Advantages: Several similar tests fall under the MBI heading; in all of them, women receive an injection of a radioactive solution that accumulates in cancerous cells more than normal cells. Then the women stand or sit with breasts slightly compressed while a scanner images them. Small studies have suggested that MBI can detect up to three times as many cancers in women with dense breast tissue and that it produces fewer false-positive results.
Caveats: MBI is still in the early stages of development and is not widely available. The radiation dose is high compared to mammography, and the injected solution also tends to accumulate in cells that are merely infected and inflamed, but not cancerous, making interpretation more challenging. MBI is not currently in use at UAB but is being considered for the near future, Umphrey says.
The Verdict
Trials of both breast MRI and MBI are under way around the country, and positive results may increase their usefulness, but they should be considered as supplements to mammography rather than replacements, Umphrey explains. “Mammography is an excellent test,” she says. “It’s not perfect, but for the foreseeable future, it will remain the gold standard.”