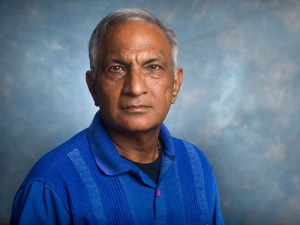
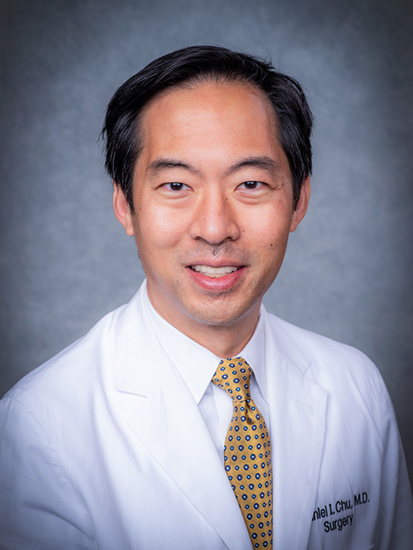
 Daniel Chu, M.D., division director of GI Surgery, leveraged an HSF-GEF grant to help Enhanced Recovery Programs reach widespread use at UAB and establish himself as a leader in the field.Surgeon Daniel Chu, M.D., knew he had a good idea. Ever since his fellowship training at the Mayo Clinic in 2013-2014, Chu had been an advocate for Enhanced Recovery Programs, or ERPs, a combination of best-evidence medical and surgical practices “that makes your recovery from major surgery better,” he said. These practices include getting patients up and walking soon after surgery, returning them to a normal diet as soon as possible, making sure they drink fluids pre- and post-surgery, and emphasizing non-opioid pain management.
Daniel Chu, M.D., division director of GI Surgery, leveraged an HSF-GEF grant to help Enhanced Recovery Programs reach widespread use at UAB and establish himself as a leader in the field.Surgeon Daniel Chu, M.D., knew he had a good idea. Ever since his fellowship training at the Mayo Clinic in 2013-2014, Chu had been an advocate for Enhanced Recovery Programs, or ERPs, a combination of best-evidence medical and surgical practices “that makes your recovery from major surgery better,” he said. These practices include getting patients up and walking soon after surgery, returning them to a normal diet as soon as possible, making sure they drink fluids pre- and post-surgery, and emphasizing non-opioid pain management.
Chu, division director of GI Surgery in the Department of Surgery, had already seen how ERPs reduced post-surgery pain and complications and gets patients moving quickly after their operations. Patients who previously would have been in bed for days post-surgery were out of bed on the same evenings after their operations and discharged in a handful of days. “It really is one of the best innovations in the 21st century for surgery,” Chu said.
After he came to UAB in 2014, Chu and Jeffrey Simmons, M.D., professor in the Department of Anesthesiology and Perioperative Medicine, collaborated to initiate an ERP pathway in colorectal surgery. On the last week of 2014, Chu performed UAB’s first ERP surgery and began growing the program with their multidisciplinary ERP team. In 2016, he, Simmons and UAB Care received a UAB Health System Innovation Award for their work. Data showed that lengths of stay after surgery, as well as pain scores, improved for colorectal surgery patients. Other service lines in the Department of Surgery began to coordinate their own ERP pathways.
In 2018, UAB Medicine partnered with SeamlessMD, which uses digital engagement technologies to improve patient engagement before and after major surgery. That includes apps for phones, tablets and computers that allow patients to learn about what to expect before and after their surgery. The app also lets them stay in constant contact with their care team to report pain scores and symptoms and send in photos of their incisions if anything concerning develops.
Enhanced Recovery Programs, or ERPs, include getting patients up and walking soon after surgery, returning them to a normal diet as soon as possible, making sure they drink fluids pre- and post-surgery. “It really is one of the best innovations in the 21st century for surgery,” Chu said.
But the gap between a pilot project in colorectal surgery and everyday use throughout the department was wide. Chu would need support to coordinate with UAB Medicine’s IT and legal teams to get SeamlessMD integrated into UAB’s electronic health record system. There was also an additional goal: Adherence to the individual components of an ERP is critical to success, Chu says, and there was early evidence that patient engagement technologies like SeamlessMD could help improve that adherence by helping patients engage with their own recovery.
So Chu applied for a grant from the UAB Health Services Foundation’s General Endowment Fund. The two-year, $210,000 HSF-GEF grant he received provided the funds to address the legal and logistical hurdles. It also allowed Chu to reach another goal: addressing the cost question. Patient technologies such as SeamlessMD clearly worked, but could they make an economic case for use? “We had good outcomes, and we were one of the first groups to show with data that the cost of installing these patient engagement technology programs is not an overall negative — in fact, it often saved money when you look at downstream savings by having shorter lengths of stay and fewer complications,” Chu said. “We have had several peer-reviewed publications come out about the cost-effectiveness and benefits of these technologies.”
“The HSF-GEF grant was absolutely critical to establishing us in this area,” Chu said. “It has catapulted us forward in terms of our research and clinical care and being at the forefront. I am very thankful."
Chu describes SeamlessMD as an early warning radar system. “I can pull up all the patients who have the app and see at a glance how they are doing,” he said. “Patients like that — it’s like an additional safety net.”
Patient engagement technologies “are here to stay,” Chu said. “We were fortunate to get in on this before it was more widely recognized, and the HSF-GEF grant was a big part of it.”
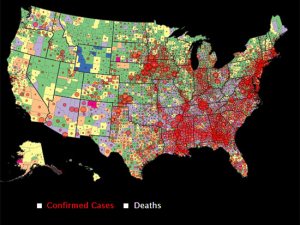
Today UAB funds the subscription costs for SeamlessMD through the Health System’s telehealth program, led by Eric Wallace, M.D. The data that Chu’s research team collects is used to apply for grants that aim to expand these programs — helping other hospitals effectively institute their own ERP pathways and patient engagement technology programs. “This is a huge piece of our work,” Chu said. “There is a whole section of research in my lab focused on patient engagement technologies and how to improve care and reduce disparities.
“The HSF-GEF grant was absolutely critical to establishing us in this area,” Chu said. “It has catapulted us forward in terms of our research and clinical care and being at the forefront. I am very thankful. It was resource-intensive up front — and that is why the grant was so helpful — but now we have a solid foundation to continue growing and making an even bigger impact on patient care.”
How do the HSF-GEF awards advance UAB? Faculty explain their projects:
How the HSF’s General Endowment Fund awards help UAB compete on a national stage
Advancing faculty careers through the UAB Academy of Health Professions Educators
Building immuno-imaging at UAB through specialized technology
Turning a pilot project into the standard of care
Making the leap from one hospital to another through UAB’s STEP Program
Building a health system that can learn calls for “team science to the max”
Using geographic information systems in patient-oriented research