Neurologist Adeel Memon, M.D., will add a Ph.D. from UAB's new neuroengineering program at the spring graduate commencement ceremony April 29. Finding a cure for neurological disorders such as Parkinson's, which affects his father, could take decades, Memon said. "But with brain-computer interfaces, we can do something now to help alleviate patients' symptoms, while the work to a cure continues." Photo by Steve WoodAdeel Memon had everything worked out.
Neurologist Adeel Memon, M.D., will add a Ph.D. from UAB's new neuroengineering program at the spring graduate commencement ceremony April 29. Finding a cure for neurological disorders such as Parkinson's, which affects his father, could take decades, Memon said. "But with brain-computer interfaces, we can do something now to help alleviate patients' symptoms, while the work to a cure continues." Photo by Steve WoodAdeel Memon had everything worked out.
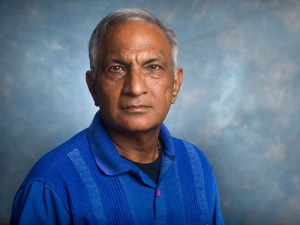
The son of a dermatologist in Karachi, Pakistan’s largest city, Memon was intent on earning the same prestigious scholarship to medical school that his father had won, becoming a dermatologist himself and joining his father’s practice. “The plan was to follow in his footsteps,” Memon said.
Memon got the scholarship, but then his father was diagnosed with Parkinson’s disease. Not coincidentally, Memon found his medical interests shifting to neurology and specifically to movement disorders, the subspecialty focused on treating conditions such as Parkinson’s, dystonia and tremor. After graduating from Dow Medical College in Karachi and finding inspiration in a viral TED Talk on YouTube about deep brain stimulation, Memon started down a new path. That led him to a neurology residency and movement disorders fellowship at UAB — and, thanks to hard work and invaluable mentors, a place on the leading edge of developing brain-computer interfaces to treat neurological conditions.
At UAB’s spring commencement April 29, Memon will add a Ph.D. to his M.D. as the first graduate of UAB’s doctoral program in neuroengineering. This joint program of the Heersink School of Medicine and School of Engineering is the only such program in Alabama and one of a handful available nationwide. But that is not Memon’s only first at UAB. He is also the nation’s first recipient of a highly competitive combined R25/Ph.D. scholarship trainee award from the National Institute of Neurological Disorders and Stroke, supporting medical residents and fellows who want to become clinician-scientists.
A “perfect fit”
In early March, Memon successfully defended his dissertation, in which he identified a correlation between cognitive impairment and three specific neural signatures in brain waves from patients with Parkinson’s disease. This summer, he will join the Department of Neurology at West Virginia University as an assistant professor. He also will start his research lab at the university’s Rockefeller Neuroscience Institute, which will be focused on “applying computations to study circuit dysfunction in movement disorders,” he said.
“We are so excited about Adeel’s being our first graduate,” said Lynn Dobrunz, Ph.D., professor in the Department of Neurobiology and co-director of the Neuroengineering Ph.D. program. “He has accomplished so much, and the work he is doing is a perfect fit with our program.”
Neuroengineering broadly defined is the application of computational and engineering techniques to problems in neuroscience, neurology and neurosurgery, Dobrunz explains. “It is highly quantitative and computational — the kind of analysis a typical neurologist wouldn’t know how to do,” she said. “There is such a need for people with this training.”
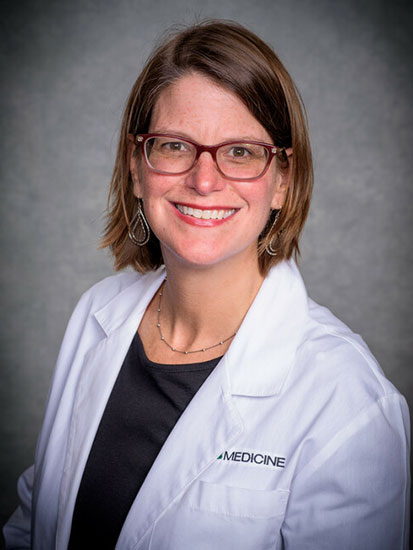
At Rockefeller, Memon will continue a close collaboration with his Ph.D. mentors Amy Amara, M.D., Ph.D., associate professor in the Department of Neurology; Zachary Irwin, Ph.D., assistant professor in the Department of Neurosurgery; and Lori McMahon, Ph.D., a longtime professor in the Department of Cell, Developmental and Integrative Biology who is now vice president for Research at the Medical University of South Carolina. Memon credits Amara, McMahon and Irwin — and the new neuroengineering doctoral program — with allowing him to fulfill his goal.
What is neuroengineering?
Neuroengineering broadly defined is the application of computational and engineering techniques to problems in neuroscience, neurology and neurosurgery, explains Lynn Dobrunz, Ph.D., professor in the Department of Neurobiology and co-director of the Neuroengineering Ph.D. program. “It is highly quantitative and computational — the kind of analysis a typical neurologist wouldn’t know how to do,” she said. “There is such a need for people with this training.” Learn more about the Neuroengineering program, including application requirements and deadlines.
Charging ahead
What’s so exciting about neuroengineering? For Memon, it is time. “Unfortunately, most neurological disorders do not have a cure and do not even have good symptomatic treatments,” Memon said. “Finding a cure could take decades. But with brain-computer interfaces, we can do something now to help alleviate patients’ symptoms, while the work to a cure continues.”
Perhaps the best example of a brain-computer interface in action today is deep brain stimulation. Neurosurgeons implant electrodes in brain regions with faulty circuits, and apply currents from an implanted battery pack in the patient’s chest to override aberrant signals. Deep brain stimulation is already widely used to reduce or eliminate tremors and other motor issues in Parkinson’s, including in patients who do not respond well to medications.
But deep brain stimulation has wider applications as well. In a spine-tingling TED Talk recorded in 2012, neurologist Michael Okun, M.D., (who trained under UAB President Ray L. Watts, M.D., at Emory University) and neurosurgeon Kelly Foote, M.D., both of the University of Florida, used patient videos to show the dramatic results that deep brain stimulation can bring about in adults with essential tremor and obsessive-compulsive disorder, and in children with dystonia. “Watching that video led me to pursue deep brain stimulation and to study circuit abnormalities,” Memon said.
On the horizon are even more breakthroughs. “By using a brain-computer interface, a user’s brain activity can be translated into commands that control an effector, such as a robotic limb, enabling patients to operate artificial limbs with their minds,” Memon said. “Deep brain stimulation is moving to closed-loop devices, which can read signatures from the brain and respond to suppress pathological signals dynamically. But a lot of work remains to apply this in patients.”
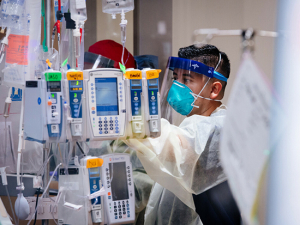
 A deep brain stimulation surgery at UAB in 2012. Photo by Steve Wood
A deep brain stimulation surgery at UAB in 2012. Photo by Steve WoodFinding a mentor
Memon aims to contribute to that work. His long-term goal is “to become a leader in intraoperative microelectrode recordings and a specialist in deep brain stimulation, and to establish a laboratory that applies computations to study circuit dysfunction in movement disorders,” he said. He always knew he could accomplish the first parts of that agenda at UAB, which is home to clinician-scientists who are internationally known for their work in deep brain stimulation and in movement disorders research.
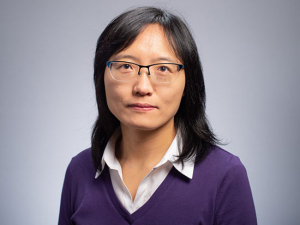
 Amy Amara, M.D., Ph.D., (above) was one of Memon's thesis advisors and Memon credits her with teaching him how to be a physician-scientist. After Memon arrived at UAB for his neurology residency, he heard department chair David Standaert, M.D., Ph.D., talk about the value of mentorship. "I had never heard of such a thing," Memon said. "But I started looking for one and found Dr. Amara."The Department of Neurology is led by David Standaert, M.D., Ph.D., a world-renowned leader in experimental treatments for movement disorders and other neurodegenerative conditions — exactly the kind of clinician-scientist that Memon wanted to become. (He was also attracted to UAB’s neurology residency program because of Professor Khurram Bashir, M.D., whom Memon describes as “the best residency director” and the other physicians in the program. “After meeting all of them, I was left with the impression that they were committed not only to providing a great learning environment but also to providing excellent care to their residents,” Memon said.)
Amy Amara, M.D., Ph.D., (above) was one of Memon's thesis advisors and Memon credits her with teaching him how to be a physician-scientist. After Memon arrived at UAB for his neurology residency, he heard department chair David Standaert, M.D., Ph.D., talk about the value of mentorship. "I had never heard of such a thing," Memon said. "But I started looking for one and found Dr. Amara."The Department of Neurology is led by David Standaert, M.D., Ph.D., a world-renowned leader in experimental treatments for movement disorders and other neurodegenerative conditions — exactly the kind of clinician-scientist that Memon wanted to become. (He was also attracted to UAB’s neurology residency program because of Professor Khurram Bashir, M.D., whom Memon describes as “the best residency director” and the other physicians in the program. “After meeting all of them, I was left with the impression that they were committed not only to providing a great learning environment but also to providing excellent care to their residents,” Memon said.)
Getting training in research was always part of Memon’s plan, although he had more enthusiasm than preparation on his CV. In Pakistan, students go straight into medical school from high school, so Memon did not have the required classes — or the funding to pursue a Ph.D. — when he first got to UAB. But that did not stop him. After he started his residency in 2015, Memon took to heart Standaert’s answer to a fellow trainee who asked about his path to success. “To become a successful physician-scientist, he said, it was essential to have a good mentor,” Memon said. “I had never heard of such a thing. I didn’t have a mentor as a medical student in Pakistan; it is a very American concept. But I started looking for one and found Dr. Amara.”
Amara is another clinician-scientist in the neurology department, with a research focus on the effects of exercise on sleep, cognitive function and other non-movement symptoms in Parkinson’s. “She knew I had no experience with research, but she still decided to take a chance on me,” Memon said. “She knew I was interested in a physician-scientist career, and I became her first graduate student. We started with baby steps, such as how to write an abstract and come up with a hypothesis. The three years I spent in Dr. Amara’s lab made me competitive to be successful in my R25 application, and I defended my thesis with data collected in her lab.”
“Adeel is a compassionate physician, a conscientious and astute scientist, and a perpetual optimist. He views obstacles as opportunities and approaches them with enthusiasm. He is extremely hardworking, kind and a pleasure to work with.” — Amy Amara, M.D., Ph.D.
“Everything fell into place”
In 2016, Standaert stopped by Memon’s research poster at the American Neurological Association annual meeting and asked about his career trajectory. When Memon said he was interested in becoming a world-class expert in deep brain stimulation, Standaert told him he needed to work with Lori McMahon, Ph.D., an acclaimed electrophysiologist and longtime director of UAB’s Comprehensive Neuroscience Center. Then, in 2017, when Standaert met with principal investigators and the NIH program manager in charge of the R25 program, the first person he encountered outside the meeting room was Memon, and Standaert suggested that he apply.
In 2019, with his R25 grant providing funding and protected time for research training, Memon began his doctoral program in neuroscience. In January of that year, he had joined McMahon’s lab to learn the techniques of slice electrophysiology in animal models of Parkinson’s disease and how to build electrodes for in-vivo recordings of the critical region of the brain known as the dorsal striatum. “At the end of the day, all of these brain circuits and interactions come down to physiology,” Memon said. “Understanding electrophysiology is critically important for the work I want to do.”
 While at UAB, Memon was selected as the nation’s first recipient of a highly competitive combined R25/Ph.D. scholarship trainee award from the National Institute of Neurological Disorders and Stroke. He also has won scholarships and memberships at national medical and scientific societies. He now has a faculty and research position at West Virginia University, where he will continue to work with UAB investigators and move toward clinical trials of techniques that could improve cognitive performance in patients with Parkinson's disease. Photo by Steve WoodThen, at an October 2019 meeting of the Comprehensive Neuroscience Center, “Dr. Dobrunz announced the new neuroengineering program and shared the curriculum,” Memon recalled. “I took a picture of that and said, ‘These are the classes I want to take, so that when the program opens, I can apply to transfer.’” The neuroengineering Ph.D. program launched in fall 2020, and Memon became its first student by transferring into the program. “Dr. Dobrunz says it was meant to be, the way everything fell into place,” Memon said.
While at UAB, Memon was selected as the nation’s first recipient of a highly competitive combined R25/Ph.D. scholarship trainee award from the National Institute of Neurological Disorders and Stroke. He also has won scholarships and memberships at national medical and scientific societies. He now has a faculty and research position at West Virginia University, where he will continue to work with UAB investigators and move toward clinical trials of techniques that could improve cognitive performance in patients with Parkinson's disease. Photo by Steve WoodThen, at an October 2019 meeting of the Comprehensive Neuroscience Center, “Dr. Dobrunz announced the new neuroengineering program and shared the curriculum,” Memon recalled. “I took a picture of that and said, ‘These are the classes I want to take, so that when the program opens, I can apply to transfer.’” The neuroengineering Ph.D. program launched in fall 2020, and Memon became its first student by transferring into the program. “Dr. Dobrunz says it was meant to be, the way everything fell into place,” Memon said.
Memon now had two of his three doctoral mentors. But he knew there was one remaining gap in his understanding: computational analysis. The data generated in a sleep study, brain scan or deep brain stimulation microelectrode recording is immense. Finding predictive relationships or patterns in that data requires specialized expertise in programming, time series analysis, linear algebra and more.
“I didn’t have the math background,” Memon said. But Irwin, his other mentor, helped him get up to speed. “He would sit down with me and say, ‘This is what we need to be doing,’” Memon said. “He is very young and establishing his own lab here at UAB, but he took the time out to help me.”
Award winner plans his next steps
While training at UAB, Memon demonstrated excellence in each of the four pillars of academic medicine, Dobrunz notes. “He twice won awards for excellence in medical student teaching and was honored as the best resident in the neurology consult service,” she said. “He was also awarded scholarships from the American Neurological Association and Movement Disorders Society for presenting his research, as well as serving as the consortium chair for residents and fellows at the American Academy of Neurology. After being inspired by Dr. McMahon’s leadership skills, he has continued to serve as a leader and is currently serving on the Executive Board of the Pakistan International Neuroscience Society. As a result of his professional achievements, he was selected as a member of the Alpha Omega Alpha Honor Medical Society.”
Now, as Memon begins his lab at the Rockefeller Institute, he will continue to collaborate with Irwin, Amara and McMahon. The brain signatures he identified in his dissertation could eventually become an early warning sign to help clinicians identify patients at risk for cognitive decline. It may also be possible to alter these brain waves through non-invasive techniques such as transcranial direct current stimulation, or tDCS, Memon says. He plans to apply for an NIH K award, proposing “to design experiments where we would be blocking or enhancing the spindle [wave] in those signatures to see if there is a causative relationship between those markers and cognition,” Memon said. “The hypothesis would be that if you enhance the spindle there would be improvement in cognitive performance in patients with Parkinson’s disease.”