2002 Case #7 |
 |
|
| Diagnosis: Intestinal perforation due to Balantidium coli infection. Secondary bacterial sepsis. |
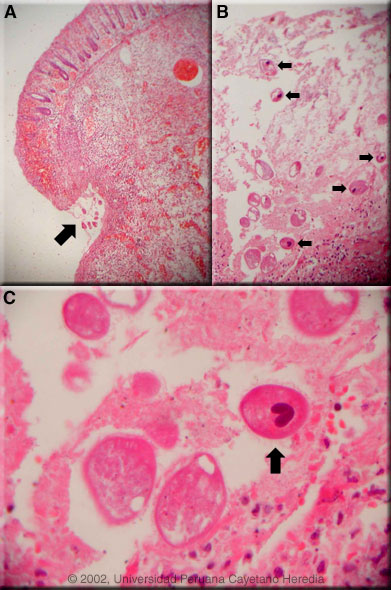 Discussion: Balantidium coli is the largest protozoan and the only ciliate parasite that infects humans. Many animal species harbor the organism as an intestinal commensal but pigs have a particularly high rate of infection and are usually considered to be the main reservoir of this organism. Panel A shows a low-power view of normal mucosa merging into hemorrhagic necrosis seen at the heaped up border of the ulcer; the arrow shows several typical Balantidium coli trophozoites at the base of the ulcer. Panel B shows a large number of Balantidium coli at higher magnification where the characteristic macronuclei can already be distinguished (arrows). Panel C shows a high power view of an organism with the characteristic kidney or sausage-shaped macronucleus. The pathognomonic cilia can also be distinguished. Trophozoites are typically more pointed at the anterior end. Rounded cyst forms can be found in stool specimens in asymptomatic cases, but in patients with clinical manifestations generally only trophozoites are found in tissue or stool. Discussion: Balantidium coli is the largest protozoan and the only ciliate parasite that infects humans. Many animal species harbor the organism as an intestinal commensal but pigs have a particularly high rate of infection and are usually considered to be the main reservoir of this organism. Panel A shows a low-power view of normal mucosa merging into hemorrhagic necrosis seen at the heaped up border of the ulcer; the arrow shows several typical Balantidium coli trophozoites at the base of the ulcer. Panel B shows a large number of Balantidium coli at higher magnification where the characteristic macronuclei can already be distinguished (arrows). Panel C shows a high power view of an organism with the characteristic kidney or sausage-shaped macronucleus. The pathognomonic cilia can also be distinguished. Trophozoites are typically more pointed at the anterior end. Rounded cyst forms can be found in stool specimens in asymptomatic cases, but in patients with clinical manifestations generally only trophozoites are found in tissue or stool.
B. coli appears to have a worldwide distribution but is considered an uncommon human infection. However, most of the literature (1,000 cases or so) is concerned with individual symptomatic or complicated cases. A small number of population-based studies including from Bolivia and Ecuador have reported prevalances of 1-6% in asymptomatic individuals in highly endemic areas. Thus, it appears that humans are quite refractory to infection with this ubiquitous porcine parasite and the factors that result in severe disease in a very small number of individuals are not clear. Our patient had no apparent underlying disease or risk factors. Interestingly, numerous attempts have been made over the years to experimentally infect humans with significant numbers of B. coli organisms isolated from various animals, but they have been unsuccessful. Transmission is thought to be via contamination of water supplies by pig feces or by direct contact with pigs. Human-to-human transmission has been reported. In the sporadic cases that have clinical manifestations, stools may be either watery or dysenteric. Fulminant disease presents rarely and is most associated with fulminating dysentery with multiple intestinal perforations, as in our case. The colonic ulcers and clinical presenation are similar to those found in amebic dysentery/peritonitis with deep invasion of submucosa with organisms. Occasional involvement of appendix and terminal ileum have been reported but this is a predominantly colonic process. The other major diagnostic consideration in a case of infectious peritonitis or intestinal perforation in this setting would be amebic disease. Pyogenic abscess due to a ruptured diverticulum or appendix or tuberculous peritonitis would have been accompanied by fever from the outset. Intestinal perforation due to typhoid fever is common in an endemic area such as Perú, but is almost always preceded by a prolonged febrile illness and is usually due to a single perforation in the ileum and not the colon. Tetracycline is generally considered to be the drug of choice, but successful therapy with metronidazole or iodoquinol has been described. The patient had a complicated post-operative course, developing DIC, acute renal failure, and ARDS, and died 2 days post-operatively. |
