| 2004 Case #1 |  |
|
| 2004 Case #1 Diagnosis& Discussion |
 |
|
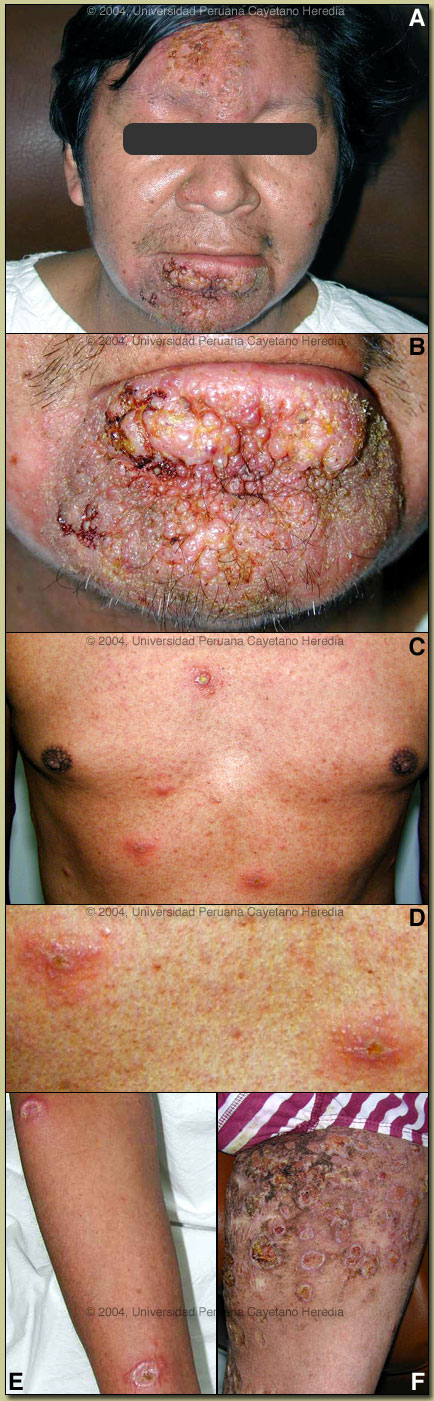
| Diagnosis: Disseminated leishmaniasis due to Leishmania braziliensis. |
| Discussion: An aspirate of an ulcerated lesion on the arm was positive for intracellular amastigotes on direct smear. Promastigotes of Leishmania were isolated from culture on NNN media of the aspirate as well as from a biopsy. PCR is pending. Cultures for fungi and AFB are negative. A leishmanin skin test was positive at 5 mm. L. braziliensis is the only leishmanial species present in this area of the jungle.
In South America it is important to distinguish Leishmania species that cause only cutaneous disease from the mucocutaneous species. Both typically cause one or a few initial skin lesions that are ulcerative but painless in nature. However, with L. braziliensis (the mucocutaneous species), severe destructive recurrence may occur in the mucosal surfaces of the naso- and oropharynx from months to years after treatment or healing of the skin ulcers. In this part of the world the vector is the Lutzomyia sandfly. Disseminated leishmaniasis (DL) is a new and emerging form of L. brasiliensis infection first reported from Brazil (J Infect Dis 2002; 186: 1829-34). Patients with DL present with 10-300 lesions that are a mixture of acneiform, ulcerative, papular, and nodular types. Approximately one quarter have mucosal involvement as well. The leishmanin skin test is usually positive. A case definition of a total of >10 mixed type lesions located in at least 2 different body parts has been proposed although most patients have a large number of body areas affected. Several cases of DL have been seen at our institute. This clinical syndrome should be distinguished from DCL or diffuse cutaneous leishmaniasis, which has been well described throughout central/south America and the Caribbean, but is usually due to L. amazonensis or L. mexicana. DCL patients have diffuse lesions which are exclusively nodular or infiltrative in nature and which are not ulcerative. Such DCL patients are anergic to leishmanial antigen and have a negative leishmanin skin test. The specific pathophysiology of DL is not yet defined. DL patients have positive leishmanin skin tests, and antigen specific cytokine production appears to be decreased though not absent as in DCL patients. DL patients are relatively refractory to therapy. To our knowledge a 20 year follow-up of the evolution of a DL case has not been reported elsewhere. Our patient received multiple but irregular and probably incomplete courses of pentavalent antimony (Glucantime) for the first 6 years. In 1993 he received 4 months of inpatient Amphotericin B which temporarily cleared all his lesions but one. He relapsed quickly, however, but did not present again for medical intervention until the recent spread to his upper body. He is presently near the end of a course of Ampotericin B at 0.6mg/kg/day to complete 2 grams of therapy. He has had partial but not dramatic resolution of his lesions so far.
|