2004 Case #4
| This past week, the annual field trip to Cusco in the Andean highlands took place. Cusco (elevation 3400m) is the oldest continuously inhabited city in the Americas. The following patient was seen on the medical ward at the Regional Hospital of Cusco. |
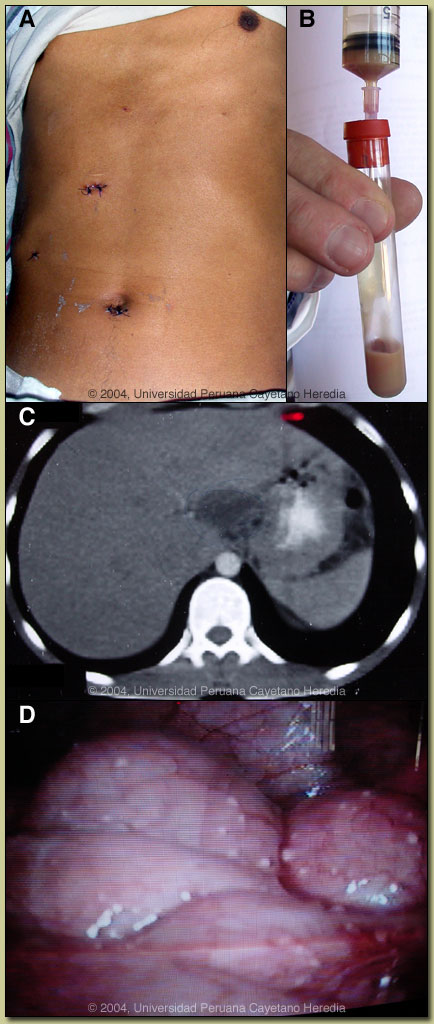 History: 29 yo previously healthy male with 4 month history of a painful fluctuant area subcutaneously over the lower sternum. Soon after he had onset of a History: 29 yo previously healthy male with 4 month history of a painful fluctuant area subcutaneously over the lower sternum. Soon after he had onset of a Epidemiology: Farmer from Sicuani in the highlands outside of Cusco. No drug or ETOH abuse. Physical Examination: Afebrile. Tender non-erythematous Laboratory Examination: Hct 45 (normal Hct at 3350m in Cusco is 55). WBC 9.1 with 57 segs, 36 lymphs. CXR normal. Sputum for AFB negative X 3. HIV negative. Needle aspirate of sternal lesion produced pus as shown in image B, which was KOH negative and gram stain negative. CT scan of the abdomen is shown in image C - besides the liver lesion the scan was otherwise unremarkable and no ascites was seen. On laparoscopy the nodules shown in image D were seen throughout the peritoneal cavity, including over the peritoneal reflections on the liver. |
| Diagnosis: Peritoneal tuberculosis with hepatic extension. |
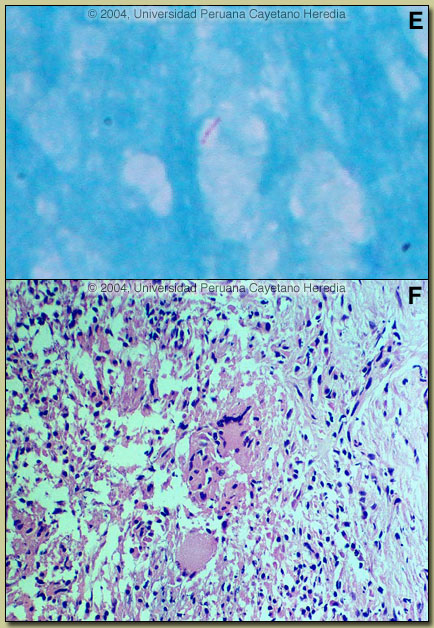 Discussion: AFB stain of the pus from the pre-sternal lesion is shown in image E. Culture is pending. Directed liver biopsy taken from the necrotic area at the time of the laparoscopy is shown in image F, and demonstrates granuloma and giant cells. Tissue AFB stain is pending. Discussion: AFB stain of the pus from the pre-sternal lesion is shown in image E. Culture is pending. Directed liver biopsy taken from the necrotic area at the time of the laparoscopy is shown in image F, and demonstrates granuloma and giant cells. Tissue AFB stain is pending.
Peritoneal tuberculosis is quite uncommon even in highly endemic countries such as Perú. Some case series show it to occur in less than 0.5% of all TB cases. Retrospective studies at our infectious disease unit in Lima show 2 or so cases per year over the past 2 decades. The diagnosis is often difficult and elusive, and often not made until tissue is obtained at laparoscopy, laparotomy, or peritoneal biopsy. CT scan when positive cannot differentiate the lesions from disseminated carcinomatosis. Ascites is present in 11-59% of cases but stain and culture of the exudative fluid is almost always unrewarding. Fever and peritoneal signs are usually present when inflammatory reaction and ascites are present. Many patients have a history of alcoholism or liver disease. No pulmonary disease is evident in more than half of patients. The pathogenesis is thought to be rupture of an infected intra-abdominal lymph node previously seeded hematogenously during an initial self-limited pulmonary infection. Peritoneal TB is distinct from intestinal TB, which is an intraluminal disease that presents with fever, diarrhea, and sometimes intestinal obstruction. This is thought to result from patients with pulmonary TB coughing up and swallowing live bacilli. Rarely, unpasteurized milk containing M. bovis is ingested and may cause intestinal disease. Therapy is the same as for pulmonary tuberculosis, and 6 month short course therapy will be used in this patient. |