| 2004 Case #5 |  |
|
| Diagnosis: Paracoccidioides brasiliensis infection (chronic form). |
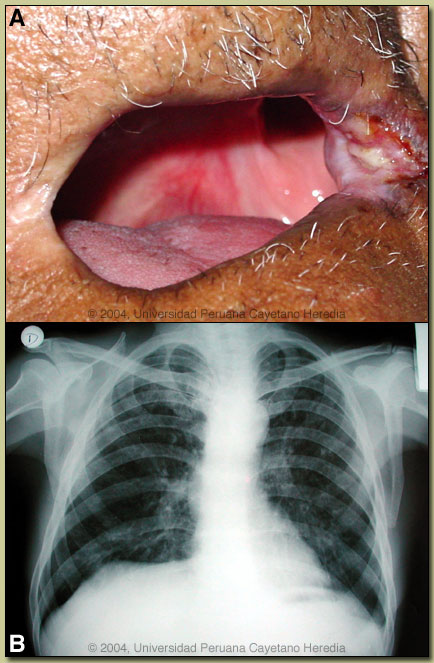
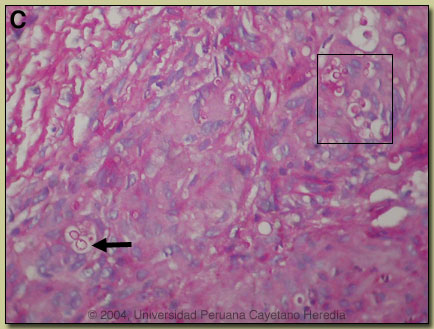 Discussion: Direct sputum examination with KOH showed P. braziliensis yeast forms with single budding. This deviation, from the typical pilot-wheel shaped organisms consisting of spherical cells 10-40 microns in diameter with a thick birefrigent cell wall surrounded by several peripheral buds, may have been caused by the prior sulfa treatment. The culture incubated at room temperature is negative so far but the filamentous forms may take up to 45 days to grow. A biopsy of the lip lesion [see image C] showed granulomas with multinucleated giant cells containing yeast forms of P. braziliensis (PAS stained; see arrow and boxed area in image). Discussion: Direct sputum examination with KOH showed P. braziliensis yeast forms with single budding. This deviation, from the typical pilot-wheel shaped organisms consisting of spherical cells 10-40 microns in diameter with a thick birefrigent cell wall surrounded by several peripheral buds, may have been caused by the prior sulfa treatment. The culture incubated at room temperature is negative so far but the filamentous forms may take up to 45 days to grow. A biopsy of the lip lesion [see image C] showed granulomas with multinucleated giant cells containing yeast forms of P. braziliensis (PAS stained; see arrow and boxed area in image).
The differential diagnosis for the lung disease includes: TB, histoplasmosis, lymphoma, cancer and cryptococcosis. The oral lesions must be differentiated from mucocutaneous leishmaniasis, TB, histoplasma, and malignancy. In general, oral lesions of paracoccidioidomycosis are painful while those of leishmaniasis are completely painless despite widespread destruction of tissue, and leishmania lesions rarely bleed. The lungs are the primary site of infection in paracoccidioidomycosis. In 30% of patients, lungs are the only organs affected, but in necropsy studies over 90% of all patients have pulmonary involvement. A characteristic clinical feature (also seen in this patient) is the dissociation between clinical symptoms and the degree of pulmonary involvement. The most typical radiographic pattern is bilateral mixed infiltrates (alveolar and interstitial), mainly located in the middle and lower lobes. Interstitial lesions may have a miliary, nodular or fibronodular patterns. This patient does not differ much from the typical pattern, although he has more upper lobe disease than expected. Other patterns observed in these patients are hilar and mediatinal lymph node enlargement, cavities, and calcified lesions. Patients with oral and skin lesions may not have respiratory symptoms, but almost always have pulmonary involvement. Extrapulmonary disease is found in over 70% of cases and may involve skin, mucous membranes, lymph nodes, adrenals, abdominal organs and CNS (in 10%). Bacterial superinfection of ulcerative lesions is more common that with oral ulcers due to mucocutaneous leishmaniasis. This case is representative of the chronic form (adult type) of the disease, which is believed to represent reactivation of latent infection. This type represents approximately 94% of all cases in the experience at our institute (94 patients, up to 2001), and approximately 85% in the Brazilian series (Rev Soc Bras Med Trop 2003;36:455-9). In our experience the male:female ratio in chronic paracoccidioidomycosis is 20:1. TB coexists in up to 10% of patients with paracoccidioidomycosis. Cavitation and pleural effusion are less commonly seen than in TB. Paracoccidioidomycosis, also known as South American blastomycosis is found in humid forested or lush green areas of the Americas from Southern Mexico south to Uruguay and Argentina. It appears to be most common in Brazil. The exact habitat of the organism is unclear but transmission is described as being entirely by airborne inhalation. However, we have observed cases with only oral lesions apparently associated with the use of tree leaves contaminated with fungal spores as toothpicks. Similarly the use of leaves as toilet paper has resulted in anal infections that can be confused with anal cancer. Primary pulmonary infection may be asymptomatic and self-limited but even with treatment will produce at least moderate pulmonary fibrosis. Rural adult males agricultural workers between 30-60 years of age are most affected by the infection. Travelers spending less than 6 months in an endemic area are unlikely to acquire paracoccidioidomycosis. Sulfonamides, ketoconazole, itraconazole, and amphotericin B are all effective therapies. Amphotericin should be reserved for severe cases. While itraconazole 100 mg/day for 6 months or so is regarded as the treatment of choice, in the developing world setting ketoconazole is likely equally effective and is usually less than half the cost. However, 12 months of therapy with ketoconazole is generally recommended. Paracoccidioidomycosis is always a severe infection that may relapse even after prolonged treatment so always needs to be treated and followed up aggressively.
|