| 2006 Case #5 |  |
|
| Diagnosis: Mucocutaneous leishmaniasis due to Leishmania braziliensis. |
 Discussion: PCR of the biopsy tissue was positive for L. braziliensis. While L. braziliensis is the only leishmanial species present in this area of the jungle, in South America it is important to definitively distinguish Leishmania species that cause only cutaneous disease (L. peruviana in Peru) from the mucocutaneous species. Both typically cause one or a few initial skin lesions that are ulcerative but painless in nature and that usually spontaneously heal over time. However, with L. braziliensis (the mucocutaneous species), severe destructive recurrence may occur in the mucosal surfaces of the naso- and oropharynx from months to years after treatment or healing of the skin ulcers. L. braziliensis only occurs in the Americas and is the only Leishmania species that causes mucocutaneous disease. In this part of the world the vector is the Lutzomyia sandfly. Discussion: PCR of the biopsy tissue was positive for L. braziliensis. While L. braziliensis is the only leishmanial species present in this area of the jungle, in South America it is important to definitively distinguish Leishmania species that cause only cutaneous disease (L. peruviana in Peru) from the mucocutaneous species. Both typically cause one or a few initial skin lesions that are ulcerative but painless in nature and that usually spontaneously heal over time. However, with L. braziliensis (the mucocutaneous species), severe destructive recurrence may occur in the mucosal surfaces of the naso- and oropharynx from months to years after treatment or healing of the skin ulcers. L. braziliensis only occurs in the Americas and is the only Leishmania species that causes mucocutaneous disease. In this part of the world the vector is the Lutzomyia sandfly.
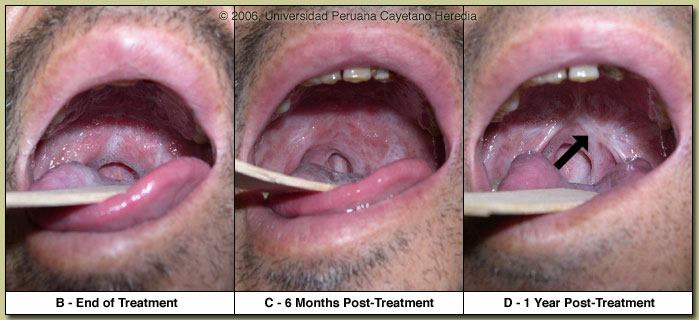
The major differential diagnosis in Peru of these oro-pharyngeal lesions would be paracoccidioidomycosis, carcinoma, or lymphoma. In Peru leishmaniasis would be by far the most common. The painless nature of the mucosal lesions despite widespread destruction of tissue, involvement of the nasal mucosa, as well as spread to the larynx are consistent only with leishmaniasis. In general, oral lesions of paracoccidioidomycosis are painful, are frequently friable and bleed on contact, and gingival and buccal mucosa are frequently involved. The lungs are the primary site of infection in paracoccidioidomycosis and the x-ray is generally abnormal. KOH preps of direct scrapings will be positive in up to 90% of cases of paracoccidioidomycosis with oral lesions. Distinguishing L. braziliensis from L. peruviana has usually involved laborious culture techniques followed by electrophoretic isoenzyme analysis. Investigators at our institute have now published a PCR assay [Clin Infect Dis. 2006 Mar 15;42(6):801-9] for distinguishing the 2 species from the initial skin lesions. Early identification of the species that causes the initial cutaneous infection would greatly help to prevent mucocutaneous leishmaniasis, because it would allow more aggressive treatment and follow-up. In Peru L. peruviana (cutaneous disease only) occurs only in the high Andes; L braziliensis occurs only in the jungle and in the Amazon. The patient received 28 days of a pentavalent antimonial (sodium stibogluconate 20mg/kg/d). He was also included in a clinical trial to evaluate the safety and immunogenicity of a vaccine (designed as an adjuvant to drug therapy) that contains 3 antigens of the parasite. In Cusco, patients such as this, with initial presentation of mucosal disease only have about a 25% response rate to antimony and are often started immediately on Amphotericin B as first line therapy. In our patient, on day 28 at the completion of therapy there was a 60% improvement in the palatal lesion [Image B], and by 1 year there was complete resolution of the lesion with some residual fibrosis [Image D]. Monitoring for failure of initial therapy is done clinically. Lesions that don?t respond at all by the end of the therapy course or don?t cure by 3 months should be considered failures and treated with another drug.
|
| This past week, the annual field trip to Cusco in the Andean highlands took place. Cusco (elevation 3400m) is the oldest continuously inhabited city in the Americas. The patient was seen at the Social Security Hospital in Cusco. We thank Dr. Maria Cruz and Dr. Alejandro Llanos for their assistance in preparing this case. |
 History: 60 yo male with a 3-year history of progressive odynophagia and dysphonia. No fever, chills, cough, weight loss or other systemic symptoms. In 1998, a small skin lesion on the chest wall persisted for 6 months before curing spontaneously. Had malaria in 1990. History: 60 yo male with a 3-year history of progressive odynophagia and dysphonia. No fever, chills, cough, weight loss or other systemic symptoms. In 1998, a small skin lesion on the chest wall persisted for 6 months before curing spontaneously. Had malaria in 1990.
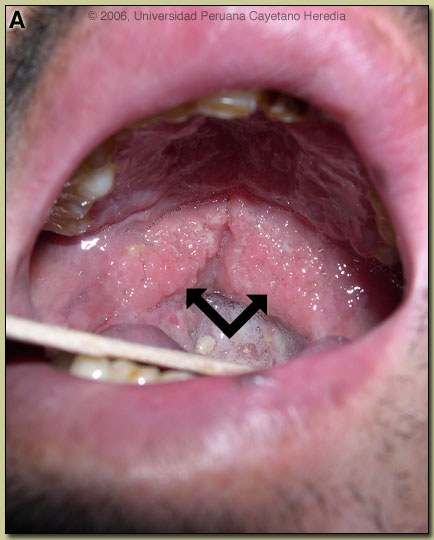
Epidemiology: Coca and coffee farmer born and living in the jungle region of Cuzco Department (6 hours from Cusco city by road). Physical Examination: Afebrile. 2 cm scar with hyperpigmented borders on the chest wall. Nasal mucosa on the right side erythematous with edema. Absent uvula, significant infiltration of the soft palatal mucosa with a granulomatous appearance [Image A]. Edema and infiltration of the epiglottis was observed under indirect laryngoscopy. Chest clear, no lymphadenopathy or organomegaly. Laboratory Examination: Hb 13.1. WBC 5.2 (47% polys, 37% lymphs), normal LFTs, stool negative for ova and parasites. Chest x-ray was normal. KOH, gram stain, and giemsa stain of direct scrapings were negative. A biopsy was taken.
|