| 2007 Case #1 |  |
|
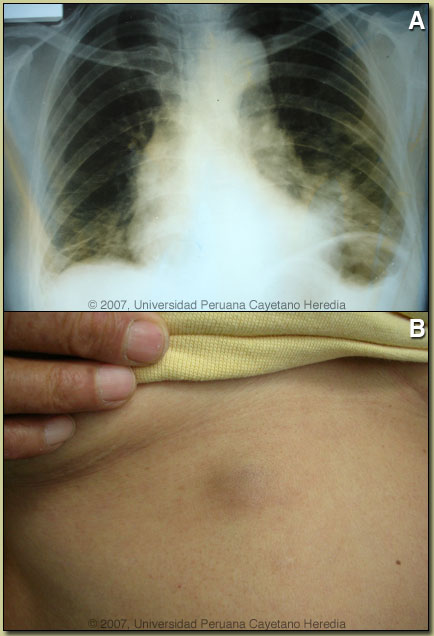
| Diagnosis: Paragonimiasis, Pulmonary and Cutaneous. |
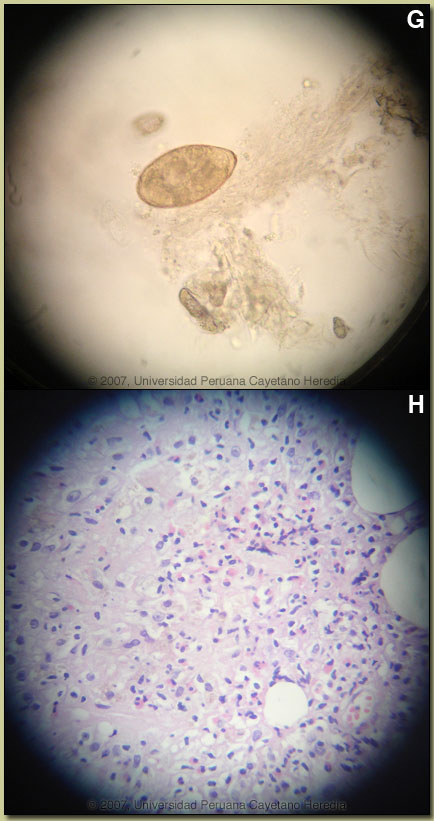 Discussion: After 4 negative tests, the fifth sputum processed and examined for ova and parasites demonstrated eggs of Paragonimus sp. [Image G]. Paragonimus eggs are destroyed in sputum being processed for acid-fast staining so sputum needs to be processed for O&P detection in order to detect eggs. Identical ova were demonstrated in the stools of our patient. Serology is not readily available. Biopsy of the skin lesion [Image H] showed fibroadipose vascularized tissue surrounding a cavity covered by granulation tissue with acute and chronic inflammation and palisading histiocytes with a tendency to form granulomas. There was a moderate eosynophilic infiltrate. Acid fast stain was negative. Discussion: After 4 negative tests, the fifth sputum processed and examined for ova and parasites demonstrated eggs of Paragonimus sp. [Image G]. Paragonimus eggs are destroyed in sputum being processed for acid-fast staining so sputum needs to be processed for O&P detection in order to detect eggs. Identical ova were demonstrated in the stools of our patient. Serology is not readily available. Biopsy of the skin lesion [Image H] showed fibroadipose vascularized tissue surrounding a cavity covered by granulation tissue with acute and chronic inflammation and palisading histiocytes with a tendency to form granulomas. There was a moderate eosynophilic infiltrate. Acid fast stain was negative.
On further questioning, the patient related that about 2.5 years ago she was feeling tired, some weakness, back pain, loss of weight, and thought she had cancer. Friends and relatives advised her to eat crabs from the local rivers, a food which she previously consumed infrequently. She began to regularly consume uncooked crab “ceviche” about 1 year before the onset of skin and respiratory symptoms. Paragonimiasis is a zoonoses caused by infection with lung flukes (trematodes) of various species. In Asia, the infection is most prevalent in China, Korea, Japan, Taiwan, and Thailand, with Paragonimus westermani the most common species. Other Asian species infecting humans include P. skrjabini, P. miyazakii, and P heterotremus. Infection in West Africa is due to P. africanus and P. uterobilateralis. In Central and South America infection is due to P. mexicanus though the nomenclature is confusing as authors in several countries have published cases as P. peruvianus and P. ecuadorensis among other names. Rigorous molecular speciation of Paragonimus in Latin America has not been performed. Adult flukes live encapsulated in cystic pockets in the lung parenchyma but may also be found in extrapulmonary locations. Parasite eggs pass into bronchi and are either coughed up into the environment or swallowed and passed in feces. On reaching fresh water they undergo an obligatory passage through a snail intermediate host and after emerging pass into a crustacean, which is a second intermediate host where they mature to infectious metacercaries which can be transmitted to humans eating undercooked crabs. The metacercariae penetrate the duodenum, pass through the diaphragm and travel to the lung parenchyma where they complete maturation. Adult flukes may live for 20 years. Clinically, patients present with cough, sputum, and progressive chest discomfort. The sputum is characteristically tenacious and gelatinous and the hemoptysis generally of a rusty brown color and not bright red. Fever is sometimes present and up to half of patients complain of some dyspnea or wheezing. Eosinophilia is often present. Cysts in the brain are more common in Asia and spinal cord disease may occur. Migratory subcutaneous nodules occur in all species but are most common in P. skrjabini. Radiologically, our patient presented in a typical fashion. With initial ill-defined opacities evolving to multiple cystic lesions. Extensive infiltrative inflammatory lesions, pleural thickening and fluid are also common. The cavities may be multilocular. The scenario presented here is common in that patients in highly TB endemic areas with hemoptysis and infiltrative lung lesions are often misdiagnosed as tuberculosis even though fever and systemic symptoms are uncommon in paragonimiasis. The patient was treated with praziquantel, the treatment of choice, 3 weeks ago and within days her respiratory symptoms and hemoptysis improved. The absolute eosinophil count has decreased to 935 at present.
|