| 2007 Case #2 |  |
|
| The following patient was seen in the inpatient department of the 36-bed Tropical Disease Unit at Cayetano Heredia National Hospital. We thank neurologist Dr. Juan Cabrera, who is caring for this patient, for his advice. |
|
History: 47-year-old male who presented to our hospital with partial motor seizures. Isolated seizures began 3 years earlier and had become weekly tonic-clonic seizures over the past several months. Oral phenytoin was begun 2 months ago after a CT scan in a peripheral hospital. After further evaluation at another hospital in Lima oral albendazole therapy was begun. Several days before the current admission the seizures worsened and post-ictally the patient exhibited bizarre behavior with frank hallucinations. There was no history of fever, cough, recent head trauma, or constitutional symptoms. Epidemiology: The patient is born and currently lives in the highlands of Ancash and owns a farm where he raises pigs, sheep, cattle, guinea pigs, dogs, cats, and donkeys. There is no history of recent travel. Frequent alcohol intake, 2-3 times per week. Physical Examination: Patient with decreased level of consciousness. BP 120/90, HR 96, RR 18, T 36.8°C. CNS: decreased level of consciousness, not oriented in time or place. Fundoscopic examination: within normal limits. Glasgow Coma Scale=12. There was nuchal rigidity with negative Kernig’s and Brudzinkis signs. Deep tendon reflexes were diminished. Remainder of exam was normal. Laboratory Examination: Chest x-ray normal. EEG normal. Electrolytes and acid-base status were normal. Hematocrit 44. WBC 9.3. Stool for ova and parasites was negative. CT scan showed multiple calcifications [Image A]. MRI was obtained [Images B, C, D].
|
| Diagnosis: Neurocysticercosis with parenchymal, intraventricular and sub-arachnoid cysts. |
Discussion: In this case, the CT and MRI scans are highly instructive as they demonstrate 4 different kinds of lesions in the same patient. The dead calcified cysticerci seen on CT scan are not seen on the later MRI which cannot detect calcification [Image A]. The parieto-occipital lesions in Image B are surrounded by significant edema indicating inflammation around a live but dying parenchymal cyst. Edema around a dying cyst is often the trigger for onset of seizures in infected individuals. Secondly, a scolex can be seen inside these lesions; visualization of a fluid filled cyst with a scolex inside is diagnostic of cysticercosis without further diagnostic or laboratory testing. Next, two cysts side by side are seen in the right ventricle [Image C]. Finally, a subarachnoid cyst, is shown by the arrow in Image D. This patient did have serology performed and the Western blot for cysticercosis was positive. 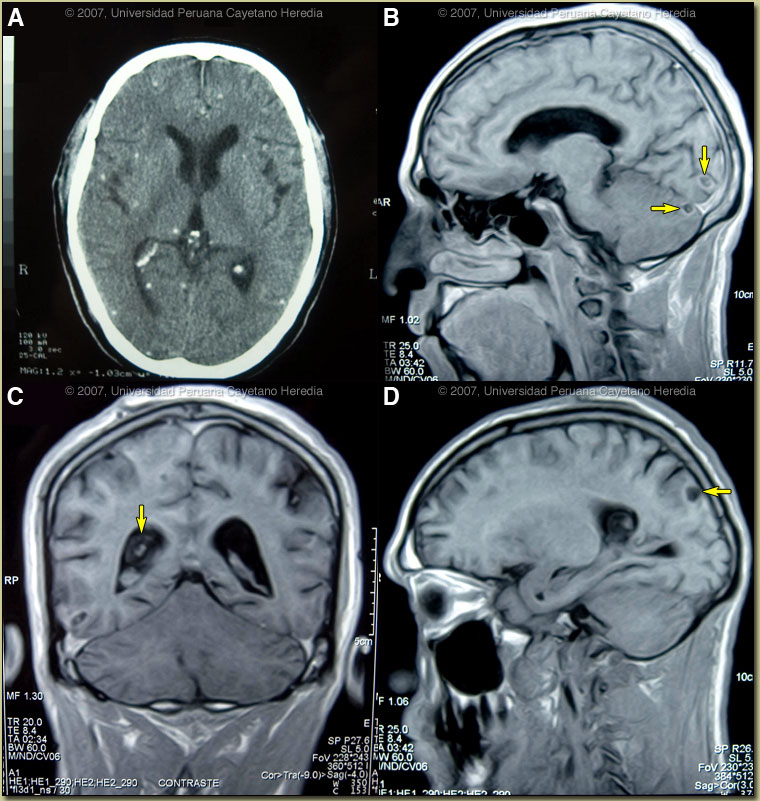
Cysticercosis is infection with the larval stages of the human pork tapeworm Taenia solium. Humans acquire cysticercosis after ingesting eggs of T. solium in material contaminated with feces originating in human tapeworm carriers. Humans that do not eat pork can get cysticercosis. Ingestion of contaminated pork results in humans getting an adult intestinal tapeworm not cysticercosis. Cysticercosis is common in many developing countries and very common in rural agricultural areas of Peru. In developed countries the long-lived cysticerci are increasingly seen as immigration from affected areas rises. Occasional transmission by tapeworm carriers to those who have never left non-endemic countries is reported. Ingested T. solium eggs hatch in the stomach and are then carried to the muscles and other tissues where the larvae encyst and reach their usual size of about 1 cm within a few months. Clinical manifestations depend on the affected organ but neurocysticercosis causes the most morbidity. The cysticerci seem able to evade the immune system and are thought to remain viable for several years without causing any inflammatory response, so that most infected patients are asymptomatic for years alter infection. Most clinical symptoms are the direct result of inflammatory responses that accompany the eventual cyst degeneration, but most patients likely remain asymptomatic even as cysts die. Epileptic seizures are the primary or sole clinical manifestation in up to 80% of symptomatic patients. In endemic regions new onset seizures in teenagers or young adults is most likely due to neurocysticercosis. Cysticerci can also cause symptoms because of mass effect, impingement on a vital structure, or blockage of CSF circulation especially if the cyst is intraventricular. In all cysticercosis patients, seizures need to be managed as per any other form of epilepsy. Treatment of parenchymal neurocysticercosis with antiparasitic drugs such as albendazole is increasingly accepted even when there are few lesions. Albendazole clearly kills the cysts, but may lead to added inflammation and exacerbation of symptoms, which is usually dealt with by empiric concomitant use of steroids. Therapeutic decisions should be based on the number, location, and viability of the cysts. Patients in whom all lesions are already calcified should receive no anti-parasitic treatment. Recent work indicates that long-standing calcified lesions can sometimes provoke peri-lesional edema, which may need treatment with steroids as well as anti-seizure medication. Separate considerations apply to patients with subarachnoid, ventricular, or intramedullary disease. This case illustrates the limitations of CT scan alone in fully assessing these patients. The CT scan in this case showed old calcified lesions and was not able to indicate the presence of the intraventricular or sub-arachnoid lesions. The presence of intraventricular lesions is an absolute contraindiction to antiparasitic chemotherapy for the reasons well illustrated here. Intraventricular inflammation due to rapid death of the cysts will exacerbate seizures and was responsible for this patient’s acute cognitive deterioration. The omission of steroids in his initial regimen also hastened his deterioration. The treatment of intraventricular disease is neuroendoscopic removal of whole cysts from the ventricle without any antiparasitic therapy. This patient was also unfortunate to have a subarachnoid cyst, which may also cause prolonged inflammation and leptomeningeal irritation after albendazole therapy and may result in a prolonged need for steroid therapy. In general, albendazole should be used in patients with sub-arachnoid cysts but more careful follow-up, in-patient admission, and a willingness to place an intraventricular drain if necessary is involved in the care of such patients. In our patient, albendazole was stopped and the patient responded well to steroids, mannitol, and anti-seizure medication. He is awaiting ventricular endoscopy.
|