| 2011 Case #1 |  |
|
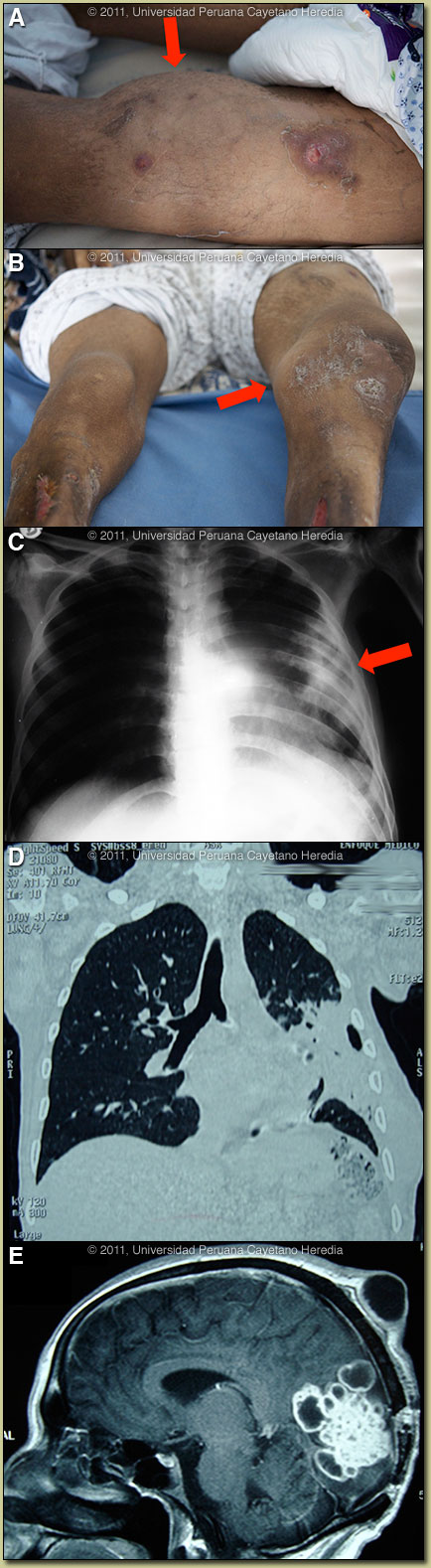
| Diagnosis: Disseminated nocardiosis. |
 Discussion: An aspirate of a right forearm abscess grew a weakly acid-fast organism compatible with Nocardia species when cultured aerobically [Images F, G]. Further workup is in progress. In addition, as aspirate of the knee joint grew Nocardia. The culture was negative for mycobacteria and did not grow anaerobically. Review of the images indicated that both the scalp and chest-wall lesions were contiguous with internal foci of infection. The brain MRI is highly diagnostic of nocardiosis. Discussion: An aspirate of a right forearm abscess grew a weakly acid-fast organism compatible with Nocardia species when cultured aerobically [Images F, G]. Further workup is in progress. In addition, as aspirate of the knee joint grew Nocardia. The culture was negative for mycobacteria and did not grow anaerobically. Review of the images indicated that both the scalp and chest-wall lesions were contiguous with internal foci of infection. The brain MRI is highly diagnostic of nocardiosis.
Although literature is limited, nocardiosis appears to present in the tropics in a similar way to non-tropical areas, though this is the first case we have seen in over 20 years in our tertiary care facility in Lima. Although M. tuberculosis infection would be at the top of the differential diagnosis list in the tropics at initial pulmonary presentation in this case, the spread to skin, joint and CNS would be unusual. Actinomycosis rarely presents in the CNS and actinomycotic skin lesions arise entirely by contiguous spread usually from a respiratory focus and that would not explain the hematogenous spread to the knee joint here. Endemic fungi (sporotrichosis, paracoccidioidomycosis) can present with skin nodules but these quickly ulcerate and would not remain nodular over a period of years. Some uncommon disseminated forms of L. brasiliensis exist but would not have pulmonary or CNS manifestations. Nocardia are aerobic, partially acid-fast, branching, filamentous, slow growing Gram-positive bacilli. Infection is acquired by direct inoculation or inhalation and spreads hematogenously from the lungs. Six basic forms of disease reported: pulmonary, systemic, central nervous system (rare), extrapulmonary, cutaneous, and actinomycetoma (often presenting as ‘madura foot’ in the tropics). Nocardiosis is mostly seen in severely immunosuppressed patients such as with HIV, organ transplantation, corticosteroid therapy, autoimmune conditions, COPD, and malignancy. TMP/SXT prophylaxis as used with many of these patients for a number of other infections does not seem highly protective against nocardiosis. The great majority of patients have a risk factor; our patient had a long history of alcoholism and incarceration. There are no therapeutic recommendations based on clinical trials. Usually, TMP/SMX is the primary choice for brain abscesses. For the disseminated form, as here, intravenous therapy should be for at least 2 months with at least 2 drugs, and with 3 drugs if there is CNS involvement. Our patient is now improving on TMP/SMX plus a third generation cephalosporin plus Amikacin. The plan is to complete oral therapy for at least 1 year.
|