| 2011 Case #10 |  |
|
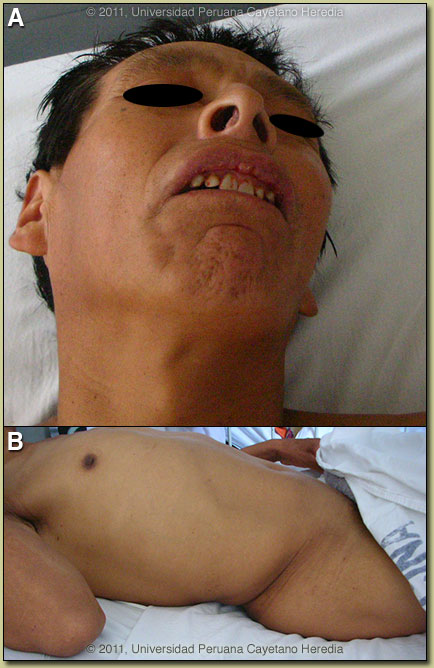
| Diagnosis: Generalized tetanus. |
 Discussion: A small wound was present [Image C] on the palmar base of the 4th finger of the right hand. Generalized tetanus is a purely clinical diagnosis with highly characteristic features, and, as in this case, the diagnosis is usually made within minutes of arrival at a medical facility. In general, disease begins with trismus or lockjaw, which are spasms of the masseter muscles, although, initial symptoms may occur in other muscle groups. After a variable period, the symptoms progress to generalized muscular rigidity, on which is superimposed increasingly severe generalized reflex muscular spasms manifested by the characteristic sardonic smile (risus sardonicus), opisthotonos (arched back), and spasm of respiratory muscles and larynx. In severe cases there are prolonged spasms occurring less than 1 hour apart, and in very severe cases there is autonomic hyperactivity with sweating, fever, tachycardia, salivation, arrhythmias, hyper- or hypotension, hyperthermia, etc. Some aspects of generalized disease can be mimicked by hypocalcemic tetany, phenothiazine induced dystonia, epilepsy, rabies, strychnine poisoning, or narcotic withdrawal, but the history of wound (not elicited in up to 20%), epidemiology, and clinical course of tetanus usually lead to little confusion. Mild localized tetanus in which trismus does not progress to generalized disease with reflex spasms is rare. In the initial phase, the trismus itself has a broader differential diagnosis including dipththeria, parotitis, odontogenic abscess, peritonsillar abscess, retropharyngeal abscess, and traumatic injury, but in these cases trismus is due to pain and there is usually fever, whereas in tetanus trismus is due to masseter rigidity and initially there is no fever. Discussion: A small wound was present [Image C] on the palmar base of the 4th finger of the right hand. Generalized tetanus is a purely clinical diagnosis with highly characteristic features, and, as in this case, the diagnosis is usually made within minutes of arrival at a medical facility. In general, disease begins with trismus or lockjaw, which are spasms of the masseter muscles, although, initial symptoms may occur in other muscle groups. After a variable period, the symptoms progress to generalized muscular rigidity, on which is superimposed increasingly severe generalized reflex muscular spasms manifested by the characteristic sardonic smile (risus sardonicus), opisthotonos (arched back), and spasm of respiratory muscles and larynx. In severe cases there are prolonged spasms occurring less than 1 hour apart, and in very severe cases there is autonomic hyperactivity with sweating, fever, tachycardia, salivation, arrhythmias, hyper- or hypotension, hyperthermia, etc. Some aspects of generalized disease can be mimicked by hypocalcemic tetany, phenothiazine induced dystonia, epilepsy, rabies, strychnine poisoning, or narcotic withdrawal, but the history of wound (not elicited in up to 20%), epidemiology, and clinical course of tetanus usually lead to little confusion. Mild localized tetanus in which trismus does not progress to generalized disease with reflex spasms is rare. In the initial phase, the trismus itself has a broader differential diagnosis including dipththeria, parotitis, odontogenic abscess, peritonsillar abscess, retropharyngeal abscess, and traumatic injury, but in these cases trismus is due to pain and there is usually fever, whereas in tetanus trismus is due to masseter rigidity and initially there is no fever.
Disease is caused by a toxin, tetanospasmin, released by Clostridium tetani that infect the wound. Spread of toxin is both retrograde through the affected axons as well as via blood to nerve endings in other parts of the body. Masseters are usually affected first due to their short axons. The action is pre-synaptic, irreversible, and blocks inhibitory neurotransmitter action leading to muscle spasm. Poor prognostic indicators include short incubation period (< 7 days) from time of the wound to onset of symptoms (4 days here), short period of onset (< 48 hours) from onset of symptoms to first reflex spasm (3 days here), and high-risk portal of entry (compound fracture, gynecologic, postoperative, intramuscular injections, and burns). Management is complex and must be done in a well-equipped Intensive Care Unit (ICU). Non-ICU care in severe cases is associated with high mortality. General principles are listed here, but detailed written dosing protocols must be available and used for most interventions.
|