| 2011 Case #9 |  |
|
| Diagnosis: Severe dengue. |
| Discussion: A dengue IgM ELISA was positive. The patient clinically deteriorated after development of the rash, with a number of episodes of significant hypotension, the platelet count dropped to 30,000 by the second hospital day, there was severe gingival bleeding, significant hematemesis (judged to be severe) and hepatic transaminases were 2X normal. On the third hospital day an abdominal ultrasound disclosed ascites and a right pleural effusion. The patient received fluids and supportive care only and recovered by day 5. A positive tourniquet test occurs in up to 50% of patients with classic dengue and in almost all patients with severe dengue. A positive tourniquet by itself may be positive with a number of other infections so is not diagnostic of dengue by itself.
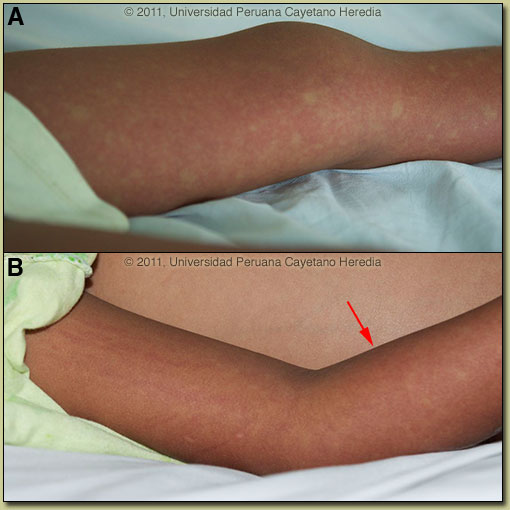
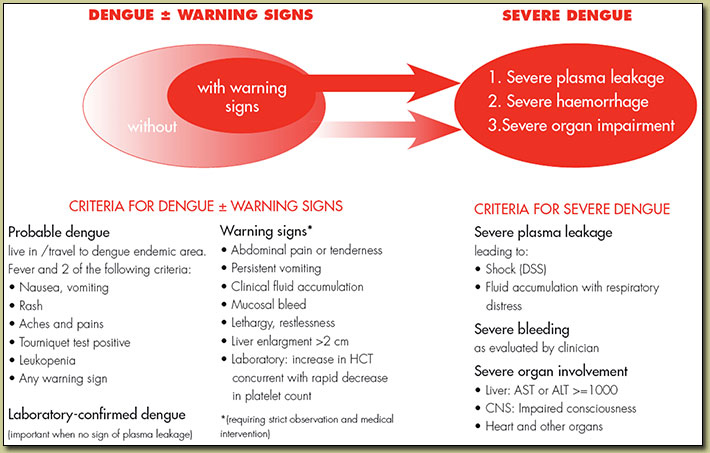
Dengue infections range from asymptomatic through a range of clinical manifestations to death. The incubation period of this flavivirus is normally 3-7 days from the time of the infective bite of the Aedes mosquito and 14 days at the most. After the incubation period, the illness begins abruptly and is followed by the three phases – febrile, critical and recovery. Typical dengue fever is manifest by frontal headache, retro-orbital pain, muscle and joint pain, nausea, vomiting and rash. The febrile phase lasts 2-7 days. An early flushlike rash often occurs and wanes after a few days to be replaced by a morbilliform rash that is often described as white islands on a red sea (as in our patient Image A). A late petechial rash may also occur. Virus may be isolated from blood; PCR of blood will be positive, or NS1 antigen may be detected in the blood during the first 5 days only. IgM elevations do not occur until 5 days or more, so a sample taken earlier may be negative. Four-fold elevations of IgG on acute and convalescent serum may be required to confirm diagnosis. When the temperature drops to 37.5–38.0ºC or less and remains below this level – usually on days 3–7 of illness – an increase in capillary permeability in parallel with increasing haematocrit levels may occur and marks the beginning of the critical phase when it occurs. This period of clinically significant plasma leakage usually lasts 24–48 hours. WHO has recently developed new criteria for dengue classification to replace the previously used clinically defined terms Classic Dengue and Dengue Hemorhagic Fever/Dengue Shock Syndrome (http://www.who.int/csr/disease/dengue/). The scheme is shown in the figure below.
Plasma leakage, haemoconcentration and abnormalities in homeostasis characterize severe dengue. The mechanisms leading to severe illness are not well defined but the immune response, the genetic background of the individual and the virus characteristics may all contribute to severe dengue. Our patient was classified as Severe Dengue because of plasma leakage leading to shock and bleeding defined as severe. Mild bleeding such as epistaxis or mucosal bleeding by itself is not enough to classify a patient as severe dengue. Increasingly, small pleural effusions are recognized in dengue by ultrasound but are not indicative of severe plasma leakage unless there is respiratory compromise. Primary infection by any of the four virus serotypes (DEN 1-4) is thought to induce lifelong protective immunity to the infecting serotype. Sero-epidemiological studies in Cuba and Thailand consistently support the role of secondary heterotypic infection (with another serotype) as a risk factor for severe dengue, although there are a number of reports of severe cases associated with primary infection, which may be a reflection of viral virulence factors. Dengue was reported in Perú for the first time in 1990; since then, all four serotypes are circulating, mainly along the north coast and the jungle. Lima was affected for the first time in 2005, with 200 cases of serotype 3 diagnosed in the northern suburban district of Comas. The Aedes vector remains present in isolated areas of the city but no further human cases have occurred. During 2011, 12,430 probable cases of dengue have been reported nationwide; almost 90% of these cases were reported from the department of Loreto and most of them from the city of Iquitos. Interestingly the case-fatality rate has increased in the city this year compared to the previous year: 1.8 per 100,000 in 2010 vs. 9.1 per 100,000 this year. A new serotype, DEN-2 Asian-American variant, has been isolated; this serotype appears more virulent than previous serotypes based on the case-fatality rate.
|